- Record: found
- Abstract: found
- Article: found
Comparison of oropharyngeal leak pressure and clinical performance of LMA ProSeal™ and i-gel® in adults: Meta-analysis and systematic review
Read this article at
Abstract
Background
A meta-analysis and systematic review of randomized controlled trials to compare the oropharyngeal leak pressure (OLP) and clinical performance of LMA ProSeal™ (Teleflex® Inc., Wayne, PA, USA) and i-gel® (Intersurgical Ltd, Wokingham, UK) in adults undergoing general anesthesia.
Methods
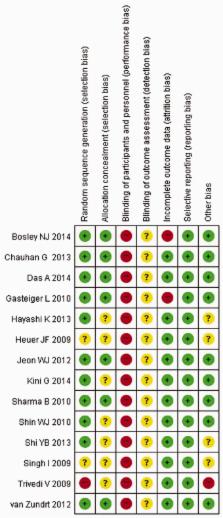
Searches of MEDLINE®, EMBASE®, CENTRAL, KoreaMed and Google Scholar® were performed. The primary objective was to compare OLP; secondary objectives included comparison of clinical performance and complications.
Results
Fourteen RCTs were included. OLP was significantly higher with LMA ProSeal™ than with i-gel® (mean difference [MD] −2.95 cmH 2O; 95% confidence interval [CI] −4.30, −1.60). The i-gel® had shorter device insertion time (MD −3.01 s; 95% CI −5.80, −0.21), and lower incidences of blood on device after removal (risk ratio [RR] 0.32; 95% CI 0.18, 0.56) and sore throat (RR 0.56; 95% CI 0.35, 0.89) than LMA ProSeal™.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients.
- Record: found
- Abstract: found
- Article: not found
Initial anatomic investigations of the I-gel airway: a novel supraglottic airway without inflatable cuff.
- Record: found
- Abstract: found
- Article: not found