- Record: found
- Abstract: found
- Article: found
Care Continuum and Postdischarge Outcomes Among HIV-Infected Adults Admitted to the Hospital in Zambia

Read this article at
Abstract
Background
We characterized the extent of antiretroviral therapy (ART) experience and postdischarge mortality among hospitalized HIV-infected adults in Zambia.
Methods
At a central hospital with an opt-out HIV testing program, we enrolled HIV-infected adults (18+ years) admitted to internal medicine using a population-based sampling frame. Critically ill patients were excluded. Participants underwent a questionnaire regarding their HIV care history and CD4 count and viral load (VL) testing. We followed participants to 3 months after discharge. We analyzed prior awareness of HIV-positive status, antiretroviral therapy (ART) use, and VL suppression (VS; <1000 copies/mL). Using Cox proportional hazards regression, we assessed risk factors for mortality.
Results
Among 1283 adults, HIV status was available for 1132 (88.2%), and 762 (67.3%) were HIV-positive. In the 239 who enrolled, the median age was 36 years, 59.7% were women, and the median CD4 count was 183 cells/mm 3. Active tuberculosis or Cryptococcus coinfection was diagnosed in 82 (34.3%); 93.3% reported prior awareness of HIV status, and 86.2% had ever started ART. In the 64.0% with >6 months on ART, 74.4% had VS. The majority (92.5%) were discharged, and by 3 months, 48 (21.7%) had died. Risk of postdischarge mortality increased with decreasing CD4, and there was a trend toward reduced risk in those treated for active tuberculosis.
Abstract
In Zambia, 86% of hospitalized HIV-infected adults were antiretroviral therapy–experienced, 50% were virally suppressed, and 71% had advanced HIV disease. Mortality within 3 months of discharge was 20%. Advanced HIV disease interventions should target inpatients in sub-Saharan Africa.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Alcohol Use and Human Immunodeficiency Virus (HIV) Infection: Current Knowledge, Implications, and Future Directions.
- Record: found
- Abstract: found
- Article: found
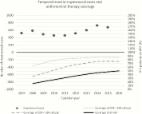
The Continuing Burden of Advanced HIV Disease Over 10 Years of Increasing Antiretroviral Therapy Coverage in South Africa
- Record: found
- Abstract: found
- Article: not found