- Record: found
- Abstract: found
- Article: found
Isolation of Acanthamoeba Spp. from Drinking Waters in Several Hospitals of Iran
Read this article at
Abstract
Background
Acanthamoeba is an opportunistic amphizoic protozoan found in different water sources including swimming pool as well as in sewage. The aim of this study was to investigate the prevalence of Acanthamoeba in tap-water samples in Iran.
Method
In this descriptive cross-sectional study, 94 samples of cold and warm tap-water were collected from different wards of hospitals in 13 cities of Iran in 2007–2008. Free residual chlorine, pH, and temperature of samples were measured. After filtration through multipore nylon membrane, samples were cultured on non-nutrient agar. Then we investigated existence of Acanthamoeba by reverse contrast phase microscope.
Results
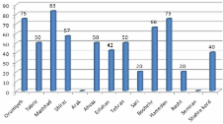
Acanthamoeba was found in 45 samples (48%). Thirty-four and 11 positive samples were collected from cold and warm tap water, respectively. The samples belonged to the category of 20–30°C temperature with 0–2 ppm free residual chlorine and pH 6–7.4 showed the most coincidence to the positive cases. The greatest proportion of positive samples was obtained from Mashhad hospitals, while all samples collected from Arak and Semnan hospitals were negative.
Conclusion
considering the results of this study and the pathogenic role of this protozoan on patients with immunodeficiency, as well as capability of this microorganism in carrying other pathogens such as Legionella, further studies are needed. What is more important, potable water in hospitals should follow the procedure of treatment and sanitation, in order to prevent the relevant nosocomial infections.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Cultivation of pathogenic and opportunistic free-living amebas.
- Record: found
- Abstract: found
- Article: not found
The hospital water supply as a source of nosocomial infections: a plea for action.
- Record: found
- Abstract: found
- Article: not found