- Record: found
- Abstract: found
- Article: found
Development of a Proficiency Testing Program for the HIV-1 BED Incidence Assay in China
Read this article at
Abstract
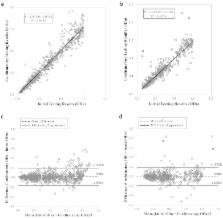
The HIV-1 BED incidence assay was adopted in China in 2005 for HIV-1 incidence surveillance. A proficiency testing (PT) program was established in 2006 to provide quality assurance services. The BED PT program consisted of two components, an international program provided by the U.S. Centers for Disease Control and Prevention from 2006 and a domestic program started by the National HIV/HCV Reference Laboratory in 2011. Each PT panel consisted of eight coded specimens distributed to participating laboratories semi-annually, and testing results were collected and analyzed. The number of participating laboratories increased progressively from 2006 to 2012. The Chinese HIV-1 incidence laboratory network performed satisfactorily both in international and domestic PT programs. We also demonstrated that the BED assay was highly reproducible among participating laboratories. Our success and lessons learned can be readily replicated in other countries or regions contemplating the establishment of a PT program for assay-based HIV incidence estimation.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Estimation of HIV incidence in the United States.
- Record: found
- Abstract: found
- Article: not found
Evolution of China's response to HIV/AIDS
- Record: found
- Abstract: found
- Article: not found