- Record: found
- Abstract: found
- Article: found
Nucleoside diphosphate-linked moiety X-type motif 15 R139C genotypes impact 6-thioguanine nucleotide cut-off levels to predict thiopurine-induced leukopenia in Crohn’s disease patients
Read this article at
Abstract
BACKGROUND
Thiopurine-induced leukopenia (TIL) is a life-threatening toxicity and occurs with a high frequency in the Asian population. Although nucleoside diphosphate-linked moiety X-type motif 15 ( NUDT15) variants significantly improve the predictive sensitivity of TIL, more than 50% of cases of this toxicity cannot be predicted by this mutation. The potential use of the 6-thioguanine nucleotide (6TGN) level to predict TIL has been explored, but no decisive conclusion has been reached. Can we increase the predictive sensitivity based on 6TGN by subgrouping patients according to their NUDT15 R139C genotypes?
AIM
To determine the 6TGN cut-off levels after dividing patients into subgroups according to their NUDT15 R139C genotypes.
METHODS
Patients’ clinical and epidemiological characteristics were collected from medical records from July 2014 to February 2017. NUDT15 R139C, thiopurine S-methyltransferase, and 6TGN concentrations were measured.
RESULTS
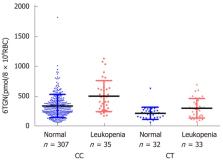
A total of 411 Crohn’s disease patients were included. TIL was observed in 72 individuals with a median 6TGN level of 323.4 pmol/8 × 10 8 red blood cells (RBC), which was not different from that of patients without TIL ( P = 0.071). Then, we compared the 6TGN levels based on NUDT15 R139C. For CC ( n = 342) and CT ( n = 65) genotypes, the median 6TGN level in patients with TIL was significantly higher than that in patients without (474.8 vs 306.0 pmol/8 × 10 8 RBC, P = 9.4 × 10 -5; 291.7 vs 217.6 pmol/8 × 10 8 RBC, P = 0.039, respectively). The four TT carriers developed TIL, with a median 6TGN concentration of 135.8 pmol/8 × 10 8 RBC. The 6TGN cut-off levels were 411.5 and 319.2 pmol/8 × 10 8 RBC for the CC and CT groups, respectively.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 1: Diagnosis and Medical Management.
- Record: found
- Abstract: not found
- Article: not found
Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 2: Current Management.
- Record: found
- Abstract: found
- Article: not found