- Record: found
- Abstract: found
- Article: found
Charged Particle and Conventional Radiotherapy: Current Implications as Partner for Immunotherapy
Read this article at
Abstract
Simple Summary
Immunotherapy provides the unprecedented opportunity to prolong the survival of cancer patients and even cure patients with previously untreatable malignancies. Preclinical and clinical studies show that standard photon-based radiotherapy and immunotherapy can synergize in order to promote both local and systemic anti-tumor immunity and that there is still ample room for improvement. Charged particle radiation is thought to have greater immunogenic potential compared to photon radiotherapy due to more lethal unrepaired damage, higher ionization density and thus more complex clustered DNA lesions. In this review, several factors determining the success of radiotherapy combined with immunotherapies, such as composition of the tumor, radiotherapy scheme and schedule, radiation dose, the type of radiation, are addressed. Furthermore, the theoretical basis, first pieces of evidences and new insights supporting a favorable immunogenicity profile of charged particle radiation are examined, including a depiction of best of knowledge for the immune-related responses triggered by charged particles and prospective clinical trials.
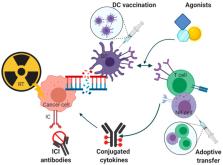
Abstract
Radiotherapy (RT) has been shown to interfere with inflammatory signals and to enhance tumor immunogenicity via, e.g., immunogenic cell death, thereby potentially augmenting the therapeutic efficacy of immunotherapy. Conventional RT consists predominantly of high energy photon beams. Hypofractionated RT regimens administered, e.g., by stereotactic body radiation therapy (SBRT), are increasingly investigated in combination with cancer immunotherapy within clinical trials. Despite intensive preclinical studies, the optimal dose per fraction and dose schemes for elaboration of RT induced immunogenic potential remain inconclusive. Compared to the scenario of combined immune checkpoint inhibition (ICI) and RT, multimodal therapies utilizing other immunotherapy principles such as adoptive transfer of immune cells, vaccination strategies, targeted immune-cytokines and agonists are underrepresented in both preclinical and clinical settings. Despite the clinical success of ICI and RT combination, e.g., prolonging overall survival in locally advanced lung cancer, curative outcomes are still not achieved for most cancer entities studied. Charged particle RT (PRT) has gained interest as it may enhance tumor immunogenicity compared to conventional RT due to its unique biological and physical properties. However, whether PRT in combination with immune therapy will elicit superior antitumor effects both locally and systemically needs to be further investigated. In this review, the immunological effects of RT in the tumor microenvironment are summarized to understand their implications for immunotherapy combinations. Attention will be given to the various immunotherapeutic interventions that have been co-administered with RT so far. Furthermore, the theoretical basis and first evidences supporting a favorable immunogenicity profile of PRT will be examined.
Related collections
Most cited references253
- Record: found
- Abstract: found
- Article: not found
PD-1 Blockade in Tumors with Mismatch-Repair Deficiency.

- Record: found
- Abstract: found
- Article: found
Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018
- Record: found
- Abstract: found
- Article: not found