- Record: found
- Abstract: found
- Article: not found
Bioavailable vitamin D is more tightly linked to mineral metabolism than total vitamin D in incident hemodialysis patients
Read this article at
Abstract
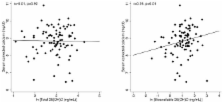
Prior studies showed conflicting results regarding the association between 25-hydroxyvitamin D (25(OH)D) levels and mineral metabolism in end-stage renal disease. In order to determine whether the bioavailable vitamin D (that fraction not bound to vitamin D binding protein) associates more strongly with measures of mineral metabolism than total levels, we identified 94 patients with previously measured 25(OH)D and 1,25-dihydroxyvitamin D (1,25(OH) 2D) from a cohort of incident hemodialysis patients. Vitamin D binding protein was measured from stored serum samples. Bioavailable 25(OH)D and 1,25(OH) 2D were determined using previously validated formulae. Associations with demographic factors and measures of mineral metabolism were examined. When compared with whites, black patients had lower levels of total, but not bioavailable, 25(OH)D. Bioavailable, but not total, 25(OH)D and 1,25(OH) 2D were each significantly correlated with serum calcium. In univariate and multivariate regression analysis, only bioavailable 25(OH)D was significantly associated with parathyroid hormone levels. Hence, bioavailable vitamin D levels are better correlated with measures of mineral metabolism than total levels in patients on hemodialysis.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Vitamin D levels and early mortality among incident hemodialysis patients.
- Record: found
- Abstract: found
- Article: not found
Vitamin D levels and patient outcome in chronic kidney disease.
- Record: found
- Abstract: found
- Article: found
