- Record: found
- Abstract: found
- Article: found
Development and Validation of a Personalized Social Media Platform–Based HIV Incidence Risk Assessment Tool for Men Who Have Sex With Men in China
Abstract
Background
Personalized risk assessments can help medical providers determine targeted populations for counseling and risk reduction interventions.
Objective
The objective of this study was to develop a social media platform–based HIV risk prediction tool for men who have sex with men (MSM) in China based on an independent MSM cohort to help medical providers determine target populations for counseling and risk reduction treatments.
Methods
A prospective cohort of MSM from Shenyang, China, followed from 2009 to 2016, was used to develop and validate the prediction model. The eligible MSM were randomly assigned to the training and validation dataset, and Cox proportional hazards regression modeling was conducted using predictors for HIV seroconversion selected by the training dataset. Discrimination and calibration were performed, and the related nomogram and social media platform–based HIV risk assessment tool were constructed.
Results
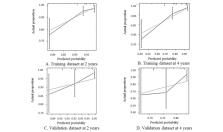
The characteristics of the sample between the training dataset and the validation dataset were similar. The risk prediction model identified the following predictors for HIV seroconversion: the main venue used to find male sexual partners, had condomless receptive or insertive anal intercourse, and used rush poppers. The model was well calibrated. The bootstrap C-index was 0.75 (95% CI 0.65-0.85) in the training dataset, and 0.60 (95% CI 0.45-0.74) in the validation dataset. The calibration plots showed good agreement between predicted risk and the actual proportion of no HIV infection in both the training and validation datasets. Nomogram and WeChat-based HIV incidence risk assessment tools for MSM were developed.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Establishment and Validation of Prognostic Nomograms for Endemic Nasopharyngeal Carcinoma
- Record: found
- Abstract: found
- Article: not found
Sexual risk, nitrite inhalant use, and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States.
- Record: found
- Abstract: found
- Article: not found