- Record: found
- Abstract: found
- Article: found
Are Opioids Needed to Treat Chronic Low Back Pain? A Review of Treatment Options and Analgesics in Development
Abstract
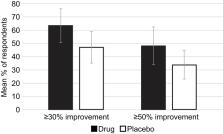
The continued prevalence of chronic low back pain (CLBP) is a testament to our lack of understanding of the potential causes, leading to significant treatment challenges. CLBP is the leading cause of years lived with disability and the fifth leading cause of disability-adjusted life-years. No single non-pharmacologic, pharmacologic, or interventional therapy has proven effective as treatment for the majority of patients with CLBP. Although non-pharmacologic therapies are generally helpful, they are often ineffective as monotherapy and many patients lack adequate access to these treatments. Noninvasive treatment measures supported by evidence include physical and chiropractic therapy, yoga, acupuncture, and non-opioid and opioid pharmacologic therapy; data suggest a moderate benefit, at most, for any of these therapies. Until our understanding of the pathophysiology and treatment of CLBP advances, clinicians must continue to utilize rational multimodal treatment protocols. Recent Centers for Disease Control and Prevention guidelines for opioid prescribing recommend that opioids not be utilized as first-line therapy and to limit the doses when possible for fear of bothersome or dangerous adverse effects. In combination with the current opioid crisis, this has caused providers to minimize or eliminate opioid therapy when treating patients with chronic pain, leaving many patients suffering despite optimal nonopioid therapies. Therefore, there remains an unmet need for effective and tolerable opioid receptor agonists for the treatment of CLBP with improved safety properties over legacy opioids. There are several such agents in development, including opioids and other agents with novel mechanisms of action. This review critiques non-pharmacologic and pharmacologic treatment modalities for CLBP and examines the potential of novel opioids and other analgesics that may be a useful addition to the treatment options for patients with chronic pain.
Most cited references89
- Record: found
- Abstract: found
- Article: not found
Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline
- Record: found
- Abstract: found
- Article: not found
Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain
- Record: found
- Abstract: found
- Article: not found