- Record: found
- Abstract: found
- Article: found
Effect of angiotensin II type 1 receptor antagonist valsartan on cardiac remodeling and left ventricular function in patients with acute ST-elevation myocardial infarction.
Read this article at
Abstract
Background: Left ventricular (LV) remodeling after acute ST-elevation myocardial infarction (STEMI) is an important predictor of mid and long-term prognosis. Pathological cardiac remodeling is associated with the development of LV systolic dysfunction and of congestive heart failure. The role of angiotensin converting enzyme (ACE) inhibitors in preventing cardiac remodeling and LV function improvement is well-known. The aim of our study was to assess the impact of an angiotensin II type 1 receptor antagonist administration instead of ACE inhibitor, in the standardized therapy of STEMI, on LV remodeling and function.
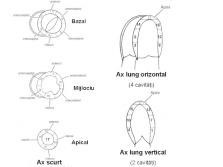
Methods: We have studied 34 consecutive patients with STEMI (91% men, mean age 58.5±10.2 years, 41% with anterior location of MI, mean GISSI class 4.7±1.2) within 6 hours of symptom onset, who received standard fibrinolytic therapy with 1.5 million IU of streptokinase, followed by unfractionated heparin for at least 48 hours. These patients also received: aspirin (100%), valsartan (100%), statins (94%), beta-blockers (85%) and other drugs according to the physician's choice. Neither of them received ACE inhibitors. An echocardiography was performed at baseline and 6 months after STEMI. Left ventricular end-diastolic diameter (LVEDD) and left ventricular mass corrected to body surface (LVm_BS) were used to assess the remodeling process. Left ventricular ejection fraction (LVEF) and a wall motion index (WMI) based on the analysis of regional contractility of 17 segments were taken into account for the LV systolic function. Changes in these values from baseline to the end of the study were compared using the Wilcoxon statistical test for paired samples.
Results: After six months follow-up, there were no significant statistical differences from baseline in LVEDD (from 52.1±6.1 to 52.7±5.6 mm, Z=0.61, p=0.53) and in LVm_BS (from 104.8±27.5 to 105.2±27.8 g/m2, Z=-0.54, p=0.54). There was a significant improvement of WMI (from 1.57±0.29 to 1.43±0.34, Z=-3.05, p=0.002) and a significant increase of LVEF (from 41.0±7.1 to 45.2±10.0%, Z=2.96, p=0.003).
Conclusions: The results of this study suggested that administration of valsartan instead of ACE inhibitor, in consecutive patients with medium-risk STEMI, attenuates pathological LV remodeling and improves LV systolic function. However, as obtained within the first six months after the infarction, these results can not be generalized to the later period after STEMI.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings.
- Record: found
- Abstract: found
- Article: not found
Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial.
- Record: found
- Abstract: found
- Article: not found