- Record: found
- Abstract: found
- Article: found
Sublingual sufentanil (Zalviso) patient-controlled analgesia after total knee arthroplasty: a retrospective comparison with oxycodone with or without dexamethasone
Abstract
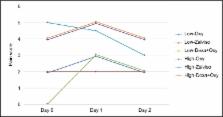
Postoperative pain is a major problem, especially in orthopedic surgery. Our data suggest suboptimal pain management after total knee arthroplasty. This study evaluated a sufentanil sublingual tablet system (Zalviso) to optimize postoperative pain treatment. This retrospective, single-center, cohort study was conducted between January 2017 and September 2017. Zalviso as standard treatment was compared with a cohort receiving oxycodone (Oxy) immediate release and Oxy extended release and another receiving Oxy immediate release, Oxy extended release, and dexamethasone (Dexa + Oxy). The primary end point, pain intensity, was assessed on a numeric rating scale (NRS). Highest, lowest, and number of NRS scores >7 were collected. Secondary end points included length of hospital stay, nausea, and mobilization on the day of surgery. Patients receiving Dexa + Oxy had a lower lowest-pain intensity on day 0 (median 0, IQR 0–0) when compared to patients receiving Oxy (median 2, IQR 0–3; P<0.0001) or Zalviso (median 2, IQR 0–4; P<0.0001). No differences were observed on day 1 or 2. No differences were observed in highest pain score or number of patients reporting NRS scores > 7. Patients treated with Dexa + Oxy or Zalviso were discharged earlier compared to patients treated with Oxy ( P<0.001). Patients treated with Zalviso experienced more nausea compared to other groups on day 0 and day 1 ( P<0.001). Patients treated with Dexa + Oxy had a higher percentage of mobilization on the day of surgery compared to Oxy and Zalviso ( P<0.001). In conclusion, Zalviso did not improve postoperative pain management in patients undergoing total knee arthroplasty and increased nausea.
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center.
- Record: found
- Abstract: found
- Article: not found