- Record: found
- Abstract: found
- Article: found
Factors affecting therapeutic compliance: A review from the patient’s perspective
Abstract
Methods
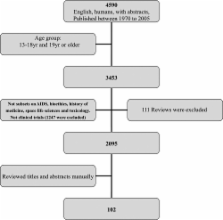
A qualitative review was undertaken by a literature search of the Medline database from 1970 to 2005 to identify studies evaluating the factors contributing to therapeutic non-compliance.
Results
A total of 102 articles was retrieved and used in the review from the 2095 articles identified by the literature review process. From the literature review, it would appear that the definition of therapeutic compliance is adequately resolved. The preliminary evaluation revealed a number of factors that contributed to therapeutic non-compliance. These factors could be categorized to patient-centered factors, therapy-related factors, social and economic factors, healthcare system factors, and disease factors. For some of these factors, the impact on compliance was not unequivocal, but for other factors, the impact was inconsistent and contradictory.
Conclusion
There are numerous studies on therapeutic noncompliance over the years. The factors related to compliance may be better categorized as “soft” and “hard” factors as the approach in countering their effects may differ. The review also highlights that the interaction of the various factors has not been studied systematically. Future studies need to address this interaction issue, as this may be crucial to reducing the level of non-compliance in general, and to enhancing the possibility of achieving the desired healthcare outcomes.
Most cited references173
- Record: found
- Abstract: found
- Article: not found
Adherence to Medication
- Record: found
- Abstract: found
- Article: not found
Social Learning Theory and the Health Belief Model
- Record: found
- Abstract: found
- Article: not found