- Record: found
- Abstract: found
- Article: found
CAT Score and SGRQ Definitions of Chronic Bronchitis as an Alternative to the Classical Definition
Abstract
Purpose
Previous studies have used various definitions to classify chronic obstructive pulmonary disease (COPD) patients into chronic bronchitis (CB) and non-CB patients. This study was performed to identify differences among three definitions of CB based on the classical method, St. George’s Respiratory Questionnaire (SGRQ), and the CAT (COPD Assessment Test) score.
Patients and methods
We extracted data from the multicenter Korea COPD Subgroup Study (KOCOSS) cohort, for which patients recruited from among 47 medical centers in South Korea beginning in April 2012. Patients were classified according to three different definitions of CB: 1) classical definition; 2) SGRQ (using questions regarding cough and sputum); and 3) CAT score (comprising cough [CAT1] and sputum [CAT2] subscale scores).
Results
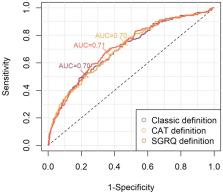
A total of 2694 patients were enrolled in this study. The proportions of CB were 10.8%, 35.8%, and 24.0% according to the classical, SGRQ, and CAT definitions, respectively. The three definitions yielded consistently significant differences between CB and non-CB patients in modified Medical Research Council dyspnea scale CAT score, SGRQ score, number of moderate-to-severe exacerbations per year and forced expiratory volume in 1 second. By three definitions, CB consistently predicted future risk of exacerbation. The kappa coefficient of agreement between the classical definition and SGRQ definition was 0.29, that of the classical definition and CAT definition was 0.32, and that of the SGRQ definition and CAT definition was 0.44.
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Susceptibility to exacerbation in chronic obstructive pulmonary disease.
- Record: found
- Abstract: not found
- Article: not found
Epidemiology Standardization Project (American Thoracic Society).
- Record: found
- Abstract: found
- Article: not found