- Record: found
- Abstract: found
- Article: found
Asthma exacerbations: prevention is better than cure
review-article
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Poorly controlled asthma is currently treated by adding or removing asthma medication in a stepwise fashion to try and improve symptoms and maintain lung function. It is becoming apparent that asthma exacerbations are independent of asthma control and severity, and that the simple method of using rescue courses of corticosteroids to treat an asthma exacerbation can be bettered by aiming to prevent its occurrence. New tools that can predict and prevent exacerbations are now becoming available. This article discusses these tools and takes a more detailed look at new treatment regimes being used.
Most cited references28
- Record: found
- Abstract: found
- Article: not found
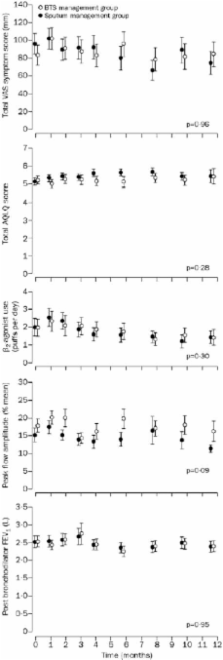
Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial.
- Record: found
- Abstract: found
- Article: not found
Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study.
Jean Bousquet, Søren Pedersen, Romain Pauwels … (2004)
- Record: found
- Abstract: found
- Article: not found