- Record: found
- Abstract: found
- Article: found
Impact of nutritional index on the association between phosphorus concentrations and mortality in haemodialysis patients: a cohort study from dialysis outcomes and practice pattern study in Japan
Read this article at
Abstract
Objectives
While maintenance of both phosphorus concentration and nutritional status is a major concern in managing haemodialysis patients, the interaction between these parameters is not well understood. The aim of this study was to assess whether or not nutritional index influences the association between phosphorus concentration and all-cause mortality.
Setting
The Dialysis Outcomes and Practice Pattern Study, which included 99 representative dialysis facilities in Japan between 1997 and 2010.
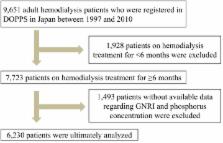
Participants
A total of 6230 adult haemodialysis patients who had spent at least 6 months on haemodialysis.
Main predictors
Six categories based on time-averaged factors of the geriatric nutritional risk index (GNRI; the lowest two and highest tertiles) and phosphorus concentration (<3.5, 3.5 to <6 and ≥6 mg/dL).
Results
During the follow-up period (12 294 person-years), we noted 561 deaths (4.6 per 100 person-years), and both high phosphorus concentrations and low-middle GNRI were separately associated with all-cause mortality. The harmful effect of high phosphorus concentrations on all-cause mortality was stronger in patients with high GNRI than in those with low-middle GNRI. On the other hand, the harmful effect of low phosphorus concentrations was stronger in those with low-middle GNRI than in those with high GNRI. Relative excess risk due to interaction (RERI) between high phosphorus concentrations and low-middle GNRI was −0.57, indicating an antagonistic interaction. We also observed a significant statistical multiplicative interaction between phosphorus concentrations and GNRI (p=0.05 by likelihood ratio test).
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients.
- Record: found
- Abstract: found
- Article: not found
A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients.
- Record: found
- Abstract: found
- Article: not found