- Record: found
- Abstract: found
- Article: found
Outcomes of 360° suture trabeculotomy with deep sclerectomy combined with cataract surgery for primary open angle glaucoma and coexisting cataract
Read this article at
Abstract
Background
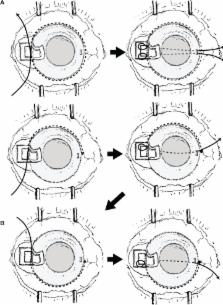
The purpose of this study was to investigate treatment outcomes in 360° suture trabeculotomy with deep sclerectomy combined with phacoemulsification and aspiration and intraocular lens implantation (360P-LOT + DS)
Methods
Thirty-two eyes in 32 consecutive patients treated by 360P-LOT + DS for primary open angle glaucoma with coexisting cataracts at Sato Eye Clinic from March 2011 to April 2013 were retrospectively compared with 23 eyes in 23 consecutive patients treated by cataract surgery and 120° trabeculotomy with deep sclerectomy (120P-LOT + DS) at the same clinic from January 2010 to February 2011. The parameters investigated during the 15 months after surgery were the course of intraocular pressure, number of antiglaucoma medications, best-corrected visual acuity, and complications.
Results
Both groups showed a significant decrease in intraocular pressure starting at one month after surgery when compared with values before surgery. At 3, 6, 9, and 15 months after surgery, the intraocular pressure was significantly lower and the survival rate was significantly higher in the 360P-LOT + DS group compared with the 120P-LOT + DS group. The number of antiglaucoma medications, best-corrected visual acuity value, and complications did not differ significantly between the groups.
Video abstract
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Cataract surgery with trabecular micro-bypass stent implantation in patients with mild-to-moderate open-angle glaucoma and cataract: two-year follow-up.
- Record: found
- Abstract: found
- Article: not found
Efficacy and safety of trabeculectomy vs nonpenetrating surgical procedures: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found