- Record: found
- Abstract: found
- Article: found
Cost of treatment: The single biggest obstacle to HIV/AIDS treatment adherence in lower-middle class patients in Mumbai, India
Read this article at
Abstract
Background:
This study analyzes the social, economic and behavioral factors most frequently associated with adherence to Highly Active Antiretroviral Treatment (HAART) in urban India.
Materials and Methods:
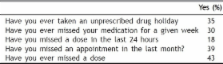
Data was collected in a metropolitan teaching hospital in Mumbai using a cross-sectional survey design. Face-to-face interviews were conducted with 152 patients. The semistructured survey included both open and closed ended questions on socio-demographic, economic and behavioral factors. Factors affecting treatment adherence were analyzed.
Results:
The median age of patients was 40.5 years, 73% were males and all were heterosexual. Patients had been given ART from six months to five years (median is equal to 3.5). Ninety per cent lived at home and commuted to the clinic by bus or train. Behaviorally, 37% were sexually active, but only 55% used condoms. In assessing adherence, income, education, knowledge of their drugs, transportation, side effects, cost of treatment, distance from clinic and personal clinic satisfaction were analyzed. We found that 75% of patients reported cost of HAART to be the single greatest obstacle to adherence (p less than 0.01). Additionally, those claiming knowledge of their drugs were 2.3 times more likely to be adherent (p less than 0.03), while those who abused drugs or alcohol were 53% less likely to be adherent (p less than 0.03). There was no correlation with other factors.
Conclusions:
Our study population was representative of the lower middle class of India. It found that an educated, employed group considered the cost of treatment to be a significant obstacle for successful therapy. Additionally, it showed a significant increase in adherence when patients had knowledge of their HAART medications. Therefore, reducing the cost of medication as well as teaching about antiretroviral medications are both likely to improve adherence.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Sociodemographic and psychological variables influencing adherence to antiretroviral therapy.
- Record: found
- Abstract: found
- Article: not found
Trust and the acceptance of and adherence to antiretroviral therapy.
- Record: found
- Abstract: found
- Article: not found