- Record: found
- Abstract: found
- Article: not found
Stroke in Africa: profile, progress, prospects and priorities

Read this article at
Abstract
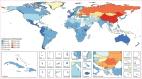
Stroke is a leading cause of disability, dementia and death worldwide. Approximately 70% of deaths from stroke and 87% of stroke-related disability occur in low-income and middle-income countries. At the turn of the century, the most common diseases in Africa were communicable diseases, whereas non-communicable diseases, including stroke, were considered rare, particularly in sub-Saharan Africa. However, evidence indicates that, today, Africa could have up to 2–3-fold greater rates of stroke incidence and higher stroke prevalence than western Europe and the USA. In Africa, data published within the past decade show that stroke has an annual incidence rate of up to 316 per 100,000, a prevalence of up to 1,460 per 100,000 and a 3-year fatality rate greater than 80%. Moreover, many Africans have a stroke within the fourth to sixth decades of life, with serious implications for the individual, their family and society. This age profile is particularly important as strokes in younger people tend to result in a greater loss of self-worth and socioeconomic productivity than in older individuals. Emerging insights from research into stroke epidemiology, genetics, prevention, care and outcomes offer great prospects for tackling the growing burden of stroke on the continent. In this article, we review the unique profile of stroke in Africa and summarize current knowledge on stroke epidemiology, genetics, prevention, acute care, rehabilitation, outcomes, cost of care and awareness. We also discuss knowledge gaps, emerging priorities and future directions of stroke medicine for the more than 1 billion people who live in Africa.
Abstract
In this Review, Akinyemi and colleagues provide an overview of stroke in Africa, including epidemiology, risk factors, genetics and available stroke services. The authors also discuss the future of stroke care in Africa, highlighting the promise of biobanking and novel leadership initiatives.
Key points
-
The annual incidence rate of stroke in Africa is up to 316 per 100,000 individuals, which is within the highest incidence rates in the world, and the prevalence rate of 1,460 per 100,000 reported in one region of Nigeria, western Africa, is clearly among the highest in the world.
-
Hypertension remains the most important modifiable risk factor for stroke in Africa but others include diabetes mellitus, dyslipidaemia, obesity, stress, smoking, alcohol use, physical inactivity and an unhealthy diet.
-
Africa has a slightly greater preponderance of small vessel disease-related stroke and intracerebral haemorrhagic lesions than elsewhere in the world.
-
The results of the first African genome-wide association study on stroke are expected soon but genes already known to modify stroke risk in African populations include IL6, APOE, APOL1, CYB11B2 and CDKN2A/2B.
-
Pragmatic approaches to improving stroke care in Africa include regular monitoring of risk factors and health services, implementation of prevention strategies, improving acute care and rehabilitation services, and encouraging task sharing; the emergence of standalone stroke care and stroke units in some North African and sub-Saharan countries is encouraging.
-
Numerous challenges face stroke medicine in Africa but awareness and the concerted efforts towards securing support for more stroke research and services via organizations such as the African Stroke Organization, World Stroke Organization and WHO hold much promise.
Related collections
Most cited references323

- Record: found
- Abstract: found
- Article: found
Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016
- Record: found
- Abstract: found
- Article: found
Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016

- Record: found
- Abstract: found
- Article: found
