- Record: found
- Abstract: found
- Article: found
Early Trends in Cystatin C and Outcomes in Patients with Cirrhosis and Acute Kidney Injury
Read this article at
Abstract
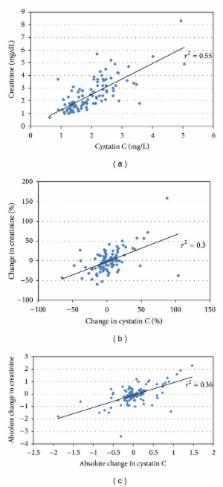
Background. Acute kidney injury (AKI) is a common and severe complication in patients with cirrhosis. Progression of AKI to a higher stage associates with increased mortality. Intervening early in AKI when renal dysfunction is worsening may improve outcomes. However, serum creatinine correlates poorly with glomerular filtration in patients with cirrhosis and fluctuations may mask progression early in the course of AKI. Cystatin C, a low-molecular-weight cysteine proteinase inhibitor, is a potentially more accurate marker of glomerular filtration. Methods. We conducted a prospective multicenter study in patients with cirrhosis comparing changes in cystatin and creatinine immediately following onset of AKI as predictors of a composite endpoint of dialysis or mortality. Results. Of 106 patients, 37 (35%) met the endpoint. Cystatin demonstrated less variability between samples than creatinine. Patients were stratified into four groups reflecting changes in creatinine and cystatin: both unchanged or decreased 38 (36%) (Scr−/CysC−); only cystatin increased 25 (24%) (Scr−/CysC+); only creatinine increased 15 (14%) (Scr+/CysC−); and both increased 28 (26%) (Scr+/CysC+). With Scr−/CysC− as the reference, in both instances where cystatin rose, Scr−/CysC+ and Scr+/CysC+, the primary outcome was significantly more frequent in multivariate analysis, P = 0.02 and 0.03, respectively. However, when only creatinine rose, outcomes were similar to the reference group. Conclusions. Changes in cystatin levels early in AKI are more closely associated with eventual dialysis or mortality than creatinine and may allow more rapid identification of patients at risk for adverse outcomes.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
Early detection of acute renal failure by serum cystatin C.
- Record: found
- Abstract: found
- Article: not found
Association of AKI with mortality and complications in hospitalized patients with cirrhosis.
- Record: found
- Abstract: found
- Article: not found