- Record: found
- Abstract: found
- Article: found
Factors associated with the health status of internally displaced persons in northern Uganda
Read this article at
Abstract
Background:
Globally, there are over 24 million internally displaced persons (IDPs) who have fled their homes due to violence and insecurity but who remain within their own country. There have been up to 2 million IDPs in northern Uganda alone. The objective of this study was to investigate factors associated with mental and physical health status of IDPs in northern Uganda.
Methods:
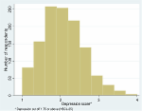
A cross-sectional survey was conducted in November 2006 in IDP camps in the Gulu and Amuru districts of northern Uganda. The study outcome of physical and mental health was measured using the SF-8 instrument, which produces physical (PCS) and mental (MCS) component summary measures. Independent demographic, socio-economic, and trauma exposure (using the Harvard Trauma Questionnaire) variables were also measured. Multivariate regression linear regression analysis was conducted to investigate associations of the independent variables on the PCS and MCS outcomes.
Results:
1206 interviews were completed. The respective mean PCS and MCS scores were 42.2 (95% CI 41.32 to 43.10) and 39.3 (95% CI 38.42 to 40.13), well below the instrument norm of 50, indicating poor health. Variables with negative associations with physical or mental health included gender, age, marital status, income, distance of camp from home areas, food security, soap availability, and sense of safety in the camp. A number of individual trauma variables and the frequency of trauma exposure also had negative associations with physical and mental health.
Related collections
Most cited references42
- Record: found
- Abstract: not found
- Article: not found
Cluster sampling to assess immunization coverage: a review of experience with a simplified sampling method.
- Record: found
- Abstract: found
- Article: not found
Mental health, social functioning, and disability in postwar Afghanistan.
- Record: found
- Abstract: found
- Article: found