- Record: found
- Abstract: found
- Article: found
Alone With the Kids: Tele-Medicine for Children With Special Healthcare Needs During COVID-19 Emergency
discussion

09 September 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
The Coronavirus Disease of 2019 (COVID-19) is a contagious respiratory illness (Sohrabi
et al., 2020) that following an initial outbreak in China is rapidly spreading worldwide.
New positive cases are increasingly identified in a growing number of countries and
the emergency has been recognized as a global pandemic (Coccia, 2020). To face and
cope with such an unprecedented healthcare emergency, National governments have adopted
specific strategies to limit the large-scale impact of the contagion (Parodi and Liu,
2020; Remuzzi and Remuzzi, 2020). Despite between-country differences exist (Chintalapudi
et al., 2020; Roux et al., 2020; Tarrataca et al., 2020), these measures have generally
changed from the initial attempts of containment to the subsequent mitigation actions.
Lockdown acts have been largely adopted to slow the virus spread, to reduce the demands
of intensive healthcare, and to control the contagion rate in the medium-long period
(Parodi and Liu, 2020).
The Fragile Condition of Families of Children with Disability During the Covid-19
Emergency
In this setting, the direct and indirect implications for citizens and healthcare
specialists have been largely highlighted (Barello and Graffigna, 2020; Barello et
al., 2020; Tian et al., 2020; Wang et al., 2020). Fragile and at-risk people—such
as children with neurodevelopmental disabilities and their parents—are especially
exposed to psychological stress related to the Covid-19 contagion and the lockdown
(Provenzi and Tronick, 2020; Provenzi et al., 2020). A major consequence of the lockdown
was the suspension of psychological and rehabilitation services for the healthcare
and educational needs of children with neurodevelopmental disability (Schiariti, 2020;
Thompson and Rasmussen, 2020). Although these children may present with different
clinical conditions—e.g., autism spectrum disorders, psychomotor delay, genetic disorders
and rare syndromes—they all share common special healthcare needs that require intensive
interventions (Wilson et al., 2014; Järvikoski et al., 2015; Giusti et al., 2018).
Italy was hit first by the Covid-19 emergency among European countries (Remuzzi and
Remuzzi, 2020) and—at the present moment—the count of positive cases is second only
to the United Kingdom. Consistently, the Italian government faced the rapid and partly
unexpected rise of the Covid-19 emergency with limited scientific, social and economic
references. After the adoption of mitigation strategies characterized by general services
lockdown, both public and local initiatives have recognized the needs of the most
fragile individuals and specific supportive services have been developed (Boldrini
et al., 2020; Leocani et al., 2020). Nonetheless, greater efforts are needed to meet
the needs of the families of children with disability (Amaral and de Vries, 2020).
Following the lockdown, parents of children with the most severe neurodevelopmental
conditions and with limited autonomy in daily activities may feel that they are left
alone in caring for their kids (Dalton et al., 2020; Thompson and Rasmussen, 2020).
The suspension of daily rehabilitation services and the lack of alternative recreational
opportunities leave these parents alone in caring for their children, with the burden
of balancing their psychosocial resources between caring for their child special needs
and accomplishing their job duties. These families have to reinvent their own space
and time organization, trying to find new ways to deal with their own needs and those
of their children. Additionally, they may partially or completely lack the support
of specialists—e.g., psychologists, educators, rehabilitation professionals, social
workers—with which they are used to engage and from which they expect to receive solutions
and relief.
Family-Centered Tele-Medicine Interventions: Bridging Physical Distancing and Assuring
Continuity of Care for Children and Parents
We live in a world where physical distances can be easily bridged by using telecommunication
devices such as personal computers, smartphones, and tablets. In order to encounter
and appropriately respond to the needs of parents of children with special healthcare
needs, specialists should invest energy and resources in tele-medicine tools and strategies
(Choon-Huat Koh and Hoenig, 2020). At the same time, policy makers and hospitals are
requested to invest in interventions based on tele-medicine in order to manage the
suspension of outpatient services and provide continuity of care (Veerapandiyan et
al., 2020). The flexible nature of the technological support allow researchers and
clinicians to develop tailored solutions that can serve different scopes: from assessment
to intervention and from parent- to child-focused activities (Figure 1). The use of
remote consultations, for example, both in the audio or video format, may be used
for children behavioral assessment (Schopp et al., 2000; Barretto et al., 2006) and
to communicate closeness, compassion and comprehension to parents while assuring quality
of care, even if in the context of mobility constraints (Follmer et al., 2010; Vismara
et al., 2013, 2018). Professionals can also share with the parents videotapes of intervention
and rehabilitation sessions that they previously registered with the child, in an
effort to provide visual examples and hints about how to pursue a continuation of
care at home (Sourander et al., 2016). Specialists and parents can also use remote
internet connections to share and co-create tools and materials to better explain
the present COVID-19 situation to children with psychomotor delay or intellectual
disability (Camden et al., 2019). Digital versions of augmentative alternative communication
symbols may allow adequate access to COVID-19-related information to children with
language impairments. Similar ad-hoc materials should be created and shared openly
with the rehabilitation community (Langkamp et al., 2015). Telephone and video-chat
connections can also serve the scope of providing parents and older children with
psychological support. As the quality of caregiving and parental well-being are known
to associate with children development (Roggman et al., 2013; Totsika et al., 2020),
providing tailored parental support during tele-medicine interventions should be considered
as a key element of the intervention itself. Notably, tele-medicine interventions
can also facilitate the direct provision of rehabilitation programs for older children
that can benefit from the on-line availability of therapeutic games and apps which
can also provide the therapists with an ongoing monitoring of the rehabilitation journey
(Corti et al., 2018; Oldrati et al., 2020).
Figure 1
Examples of different telemedicine solutions defined in terms of focus (parents, children)
and goal (assessment, intervention).
Such a family-centered approach to tele-medicine in child neuropsychiatry is warranted
to provide positive effects for both children and families (Figure 2). On the child-side,
by promoting continuity of care the risk of disrupting daily and weekly routines is
reduced and children can maintain social and affective contacts with their therapists
and specialists. Moreover, on-line rehabilitation programs can support the achievement
of developmental milestones in behavioral, cognitive and social abilities (Langkamp
et al., 2015; McConnochie et al., 2015; Knutsen et al., 2016). As parents' role in
facilitating the rehabilitation interventions is much more prominent in online interventions,
they can be more actively engaged by therapists (Myers et al., 2017; Ray et al., 2017).
Additionally, parents can receive psychological and educational support to meet their
own needs and those of their children (Harper, 2006; Hinton et al., 2017). Finally,
by actively engaging in remote therapies and rehabilitation sessions they can increase
their sense of agency and self-efficacy in parenting.
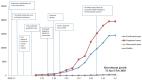
Figure 2
The potential benefits of family-centered tele-medicine for parents of children with
neurodevelopmental disabilities. The horizontal axis represents the time frame of
benefits, whereas the vertical axis represents the different positive effects for
the parents and the child.
Insights From an Ongoing Italian Family-Centered Tele-Medicine Program During the
Covid-19 Lockdown
Soon after the start of the lockdown phase in Italy, a family-centered tele-medicine
program—namely, the Engaging with Families in On-line Rehabilitation of Children during
the Epidemic (EnFORCE) program—was launched at the Child Neurology and Psychiatry
Unit of the IRCCS Mondino Foundation, in Pavia. This hospital is located in the primary
hotspot of Covid-19 spread in Italy and receives patients from the surrounding Lombardia
region as well as from other regions. The EnFORCE program was aimed at providing families
of children with neurodevelopmental disabilities that were already enrolled in outpatient
activities with an immediate tele-medicine support, reducing the risk of emotional
distress and psychological burnout during the lockdown phase. The majority of rehabilitation
interventions that were planned or ongoing for the physical setting were modified
in order to be at least partially delivered on-line, engaging parents and promoting
a positive rehabilitation partnership with therapists and healthcare professionals.
The primary aim was promoting continuity of care for children; nonetheless, a secondary
goal was providing emotional and psychological support to the parents during an unprecedented
challenging time. More than 80 families were enrolled in the study. The preliminary
findings suggest that although none of the included parents had been positive to Covid-19,
half of them were living in a high-contagion rate geographical area and up to 20%
had experienced the loss of a loved one. Concerns for the child health and the continuity
of rehabilitation programs were among the greatest sources of emotional distress for
these parents, confirming the psychological burden of lockdown in families of children
with disability. At the present moment, the intervention is ongoing and data on the
reduction of parents' psychological burden are not available. Nonetheless, all the
eligible families accepted to be enrolled in the intervention with almost 100% of
participation to the on-line sessions, which suggests that the EnFORCE program was
well-received by parents.
Challenges for Family-Centered Tele-Medicine
Tele-medicine implies also some specific critical aspects to manage. First, relevant
challenges regard the security and safety of data management and families' privacy.
Tele-medicine intervention require the shift of data storage and access on cloud services.
While this has the advantage of being convenient (e.g., complete patient history can
be available in real-time) and cost-effective (Esposito et al., 2018), cloud deployments
in healthcare industry are vulnerable to threats posed by both external attacks and
service providers. Cryptographic systems, such as block-chain technology, offer flexible
and efficient solutions (Guo et al., 2019). Moreover, policies for data management
security and protection differ between countries. The regulation concerning data ownership
and datacentre locations can be conflicting in different states and even within the
European Union there may be different degrees of control and limitations to healthcare
data storage, sharing and management (Currie and Seddon, 2014; Esposito et al., 2018).
Second, although smartphones, computers and tablets are thought to be generally available
to most of the families, demographic data only partially support this common sense
view. A recent survey conducted in the biennium 2018–2019 by the Italian National
Institute of Statistics (ISTAT)
1
revealed that approximately the 33% of families had no computer or tablet at home;
this estimates was lower (14%) for families with at least one child. Only 22% of families
had a one-to-one member-device ratio and families with low socio-economic status were
especially lacking the availability of computers and tablets. With the growing digitalization
of healthcare (Mishon et al., 2020; Moro Visconti and Morea, 2020), the availability
of technological devices in home environments becomes a key requirement for accessing
healthcare services and governments need to provide adequate economic support to promote
equality and reduce socio-economic disparities. Finally, the rehabilitation materials
and methods need to be at least partially adapted to the tele-medicine settings. This
adaptation also regards the specialist-parent relationship. Indeed, clinicians usually
have a primary role in the direct management of the rehabilitation activities, while
parents are often left on the bench. In tele-medicine settings, the therapists are
outside of the family physical space and the development of an optimal partnership
with the parents becomes both a key goal and a crucial proxy for the success of the
rehabilitation program itself.
Conclusions
The COVID-19 pandemic is asking specialists in the field of child neuropsychiatry
and rehabilitation to at least partially shift to tele-medicine programs. Nonetheless,
this unprecedented period of healthcare and socio-economic crisis can also become
an opportunity (Provenzi and Barello, 2020). Indeed, by improving our ability to use
innovative technologies to respond to the special healthcare needs of children with
disability and their families, we may proceed forward to build more inclusive societies
and smarter healthcare systems. In other words, tele-medicine strategies in developmental
neuropsychiatry should not be considered as an emergency response only. Rather, as
tele-medicine makes healthcare services accessible by underserved and resource-constrained
communities (Andreassen and Dyb, 2010; Khilnani et al., 2020), this is an unmissable
occasion to create new bridges to reduce inequalities in healthcare for children and
families. Even when we will be able to consider this emergency passed, tele-medicine
solutions are warranted to be a positive heritage of our virtuous response to the
current pandemic.
Author Contributions
LP conceived the initial draft of this work. SG drafted the final version of the work.
RB provided scientific supervision. All authors contributed to this work and agreed
on the submission of the final manuscript version.
Mondino EnFORCE Group Members
Valentina Aramini, Ilaria Baschenis, Angela Berardinelli, Laura Bernasconi, Luca Capone,
Camilla Caporali, Adriana Carpani, Stefano Cassola, Matteo Chiappedi, Raissa Francesca
Costantino, Erika Dargenio, Valentina De Giorgis, Federica Ferro, Alice Gardani, Antonella
Luparia, Chiara Magni, Martina Mensi, Cecilia Naboni, Simona Orcesi, Elena Saligari,
Sabrina Signorini, Martina Tosi, Valeria Vacchini, Costanza Varesio, Elena Vlacos,
Martina Zanaboni.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial
or financial relationships that could be construed as a potential conflict of interest.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: found
Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China
Cuiyan Wang, Riyu Pan, Xiaoyang Wan … (2020)
- Record: found
- Abstract: found
- Article: found
World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19)
Catrin Sohrabi, Zaid Alsafi, Niamh O'Neill … (2020)
- Record: found
- Abstract: found
- Article: not found
COVID-19 and Italy: what next?
Andrea Remuzzi, Giuseppe Remuzzi (2020)