- Record: found
- Abstract: found
- Article: found
A Machine Learning–Based Algorithm for the Prediction of Intensive Care Unit Delirium (PRIDE): Retrospective Study
Abstract
Background
Delirium frequently occurs among patients admitted to the intensive care unit (ICU). There is limited evidence to support interventions to treat or resolve delirium in patients who have already developed delirium. Therefore, the early recognition and prevention of delirium are important in the management of critically ill patients.
Objective
This study aims to develop and validate a delirium prediction model within 24 hours of admission to the ICU using electronic health record data. The algorithm was named the Prediction of ICU Delirium (PRIDE).
Methods
This is a retrospective cohort study performed at a tertiary referral hospital with 120 ICU beds. We only included patients who were 18 years or older at the time of admission and who stayed in the medical or surgical ICU. Patients were excluded if they lacked a Confusion Assessment Method for the ICU record from the day of ICU admission or if they had a positive Confusion Assessment Method for the ICU record at the time of ICU admission. The algorithm to predict delirium was developed using patient data from the first 2 years of the study period and validated using patient data from the last 6 months. Random forest (RF), Extreme Gradient Boosting (XGBoost), deep neural network (DNN), and logistic regression (LR) were used. The algorithms were externally validated using MIMIC-III data, and the algorithm with the largest area under the receiver operating characteristics (AUROC) curve in the external data set was named the PRIDE algorithm.
Results
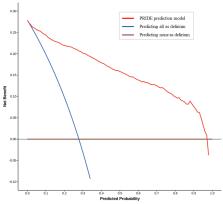
A total of 37,543 cases were collected. After patient exclusion, 12,409 remained as our study population, of which 3816 (30.8%) patients experienced delirium incidents during the study period. Based on the exclusion criteria, out of the 96,016 ICU admission cases in the MIMIC-III data set, 2061 cases were included, and 272 (13.2%) delirium incidents occurred. The average AUROCs and 95% CIs for internal validation were 0.916 (95% CI 0.916-0.916) for RF, 0.919 (95% CI 0.919-0.919) for XGBoost, 0.881 (95% CI 0.878-0.884) for DNN, and 0.875 (95% CI 0.875-0.875) for LR. Regarding the external validation, the best AUROC were 0.721 (95% CI 0.72-0.721) for RF, 0.697 (95% CI 0.695-0.699) for XGBoost, 0.655 (95% CI 0.654-0.657) for DNN, and 0.631 (95% CI 0.631-0.631) for LR. The Brier score of the RF model is 0.168, indicating that it is well-calibrated.
Conclusions
A machine learning approach based on electronic health record data can be used to predict delirium within 24 hours of ICU admission. RF, XGBoost, DNN, and LR models were used, and they effectively predicted delirium. However, with the potential to advise ICU physicians and prevent ICU delirium, prospective studies are required to verify the algorithm’s performance.
Related collections
Most cited references30

- Record: found
- Abstract: found
- Article: found
MIMIC-III, a freely accessible critical care database
- Record: found
- Abstract: found
- Article: not found