- Record: found
- Abstract: found
- Article: found
Mesenteric lymphadenitis as a presenting feature of Whipple’s disease
Read this article at
Abstract
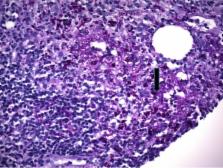
Detecting Whipple’s disease, a “great imitator”, requires a high index of suspicion so that antimicrobial treatment can be initiated in a timely manner; a missed diagnosis can be fatal. Although an uncommon cause, Whipple’s disease must be considered in adults with mesenteric lymphadenitis. We report the case of a 39-year-old African American man who presented with chronic joint pain, chronic weight loss, and acute onset epigastric pain. Contrast-enhanced computed tomography of the abdomen and pelvis showed extensive mesenteric lymphadenopathy. A diagnosis of Whipple’s disease was made based upon demonstration of PAS-positive macrophages in the mesenteric lymph node and duodenal biopsies. Antimicrobial therapy resulted in weight gain and resolution of abdominal pain and arthralgia at six months follow-up.
Whipple’s disease can be fatal without antibacterial therapy and it always needs to be considered in individuals presenting with any combination of abdominal pain, weight loss, and diarrhea in the background of nonspecific arthritis or arthralgia. Whipple’s disease must also be considered in adults presenting with mesenteric lymphadenitis. Review of CT scans may be helpful, as Whipple’s disease characteristically causes low attenuation mesenteric lymphadenopathy.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Systemic Tropheryma whipplei: clinical presentation of 142 patients with infections diagnosed or confirmed in a reference center.
- Record: found
- Abstract: found
- Article: not found
Whipple disease. Clinical review of 52 cases. The SNFMI Research Group on Whipple Disease. Société Nationale Française de Médecine Interne.
- Record: found
- Abstract: found
- Article: not found