- Record: found
- Abstract: found
- Article: found
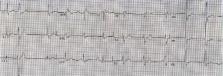
Acute chest pain after bench press exercise in a healthy young adult
Read this article at
Abstract
Bench press exercise, which involves repetitive lifting of weights to full arm extension while lying supine on a narrow bench, has been associated with complications ranging in acuity from simple pectoral muscle strain, to aortic and coronary artery dissection. A 39-year-old man, physically fit and previously asymptomatic, presented with acute chest pain following bench press exercise. Diagnostic evaluation led to the discovery of critical multivessel coronary occlusive disease, and subsequently, highly elevated levels of lipoprotein (a). Judicious use of ancillary testing may identify the presence of “high-risk” conditions in a seemingly “low-risk” patient. Emergency department evaluation of the young adult with acute chest pain must take into consideration an extended spectrum of potential etiologies, so as to best guide appropriate management.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Lipoprotein (a): truly a direct prothrombotic factor in cardiovascular disease?
- Record: found
- Abstract: found
- Article: not found
Acute myocardial infarction in the young--The University of Michigan experience.
- Record: found
- Abstract: found
- Article: not found