- Record: found
- Abstract: found
- Article: found
Balloon-Occluded Retrograde Transvenous Obliteration for Gastric Variceal Bleeding: Its Feasibility Compared with Transjugular Intrahepatic Portosystemic Shunt
Read this article at
Abstract
Objective
To assess the feasibility of balloon-occluded retrograde transvenous obliteration (BRTO) in active gastric variceal bleeding, and to compare the findings with those of transjugular intrahepatic portosystemic shunt (TIPS).
Materials and Methods
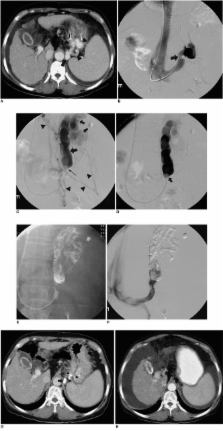
Twenty-one patients with active gastric variceal bleeding due to liver cirrhosis were referred for radiological intervention. In 15 patients, contrast-enhanced CT scans demonstrated gastrorenal shunt, and the remaining six (Group 1) underwent TIPS. Seven of the 15 with gastrorenal shunt (Group 2) were also treated with TIPS, and the other eight (Group 3) underwent BRTO. All patients were followed up for 6 to 21 (mean, 14.4) months. For statistical inter-group comparison of immediate hemostasis, rebleeding and encephalopathy, Fisher's exact test was used. Changes in the Child-Pugh score before and after each procedure in each group were statistically analyzed by means of Wilcoxon's signed rank test.
Results
One patient in Group 1 died of sepsis, acute respiratory distress syndrome, and persistent bleeding three days after TIPS, while the remaining 20 survived the procedure with immediate hemostasis. Hepatic encephalopathy developed in four patients (one in Group 1, three in Group 2, and none in Group 3); one, in Group 2, died while in an hepatic coma 19 months after TIPS. Rebleeding occurred in one patient, also in Group 2. Except for transient fever in two Group-3 patients, no procedure-related complication occurred. In terms of immediate hemostasis, rebleeding and encephalopathy, there were no statistically significant differences between the groups ( p > 0.05). In Group 3, the Child-Pugh score showed a significant decrease after the procedure ( p = 0.02).
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients.
- Record: found
- Abstract: found
- Article: not found
Prediction of variceal hemorrhage by esophageal endoscopy.
- Record: found
- Abstract: found
- Article: not found