- Record: found
- Abstract: found
- Article: found
American Academy of Pediatrics 2014 Bronchiolitis Guidelines: Bonfire of the Evidence
editorial

12 January 2015
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
A BONFIRE OF THE EVIDENCE
The American Academy of Pediatrics (AAP) 2014 Bronchiolitis guidelines (the guidelines)
were recently published in the official journal of the AAP, Pediatrics.1 The committee
that wrote the guidelines anticipates that these will form the basis of bronchiolitis
treatment throughout the house of medicine, not just in pediatricians’ offices. Emergency
physicians may well encounter pressure to follow these guidelines from their pediatric
colleagues who, not unreasonably, rely on guidelines from their professional organization.
However, two key recommendations in these guidelines could substantially change pediatric
emergency medicine practice. These recommendations are (1) to not use even a trial
of bronchodilators and (2) to regard oxygen saturations of 90% rather than 92%–94%
as the degree of hypoxia at which oxygen should be administered.1 Neither of these
recommendations is sufficiently justified by the evidence and both are potentially
harmful. We deal first with the new guideline to not use bronchodilators.
The committee bases its recommendation to not attempt even a trial of bronchodilators
on the following:
The committee’s interpretation of a meta-analysis that reported a decrease in hospital
admissions when epinephrine rather than placebo was given in the emergency department
(ED).1
A meta-analysis contained in a Cochrane review, which did not show decreased hospital
admissions from the ED when albuterol rather than placebo was given.2
Albuterol non-responders cannot be distinguished from responders, and clinicians’
ability to observe a clinically relevant response to bronchodilators is limited.1
Albuterol’s risks and expense outweigh its benefits.1
We deal with each of these in turn. Bronchiolitis causes lower airway obstruction
through a combination of bronchiolar obstruction with inflammatory cells, cellular
debris, increased mucus secretion, and varying degrees of bronchospasm. This combination
has prompted treatment with nebulized epinephrine, which can decrease mucosal edema
and has bronchodilator properties, and albuterol, which is best known for its bronchodilator
properties (Footnote[a]).3–5
A meta-analysis found a decrease in hospital admissions from the ED risk ratio 0.67
(95% CI [0.50–0.89]) favoring epinephrine over placebo.6 This analysis was heavily
influenced by Plint et al., which recruited 800 patients divided into four groups
comparing combinations of epinephrine, saline, dexamethasone, and placebo and found
early benefits but little difference at one week between nebulized epinephrine and
normal saline.7 Both this meta-analysis and Plint et al. were published by the same
group, and as reported the meta-analysis would have justified further funding for
additional studies.6
However, this meta-analysis excluded another large randomized controlled trial (RCT)
comparing albuterol and epinephrine.6 Walsh et al. randomized 703 patients in two
groups comparing nebulized albuterol and epinephrine.83 This study found a relative
increase in ED discharge of 18% when albuterol rather than epinephrine was used (aRR
1.18 for successful ED discharge without admission at three days follow up).8 This
is equivalent to a risk ratio of 0.86 (95% CI [0.76–0.98]) for decreased admission.
Since an adequately powered large RCT had already demonstrated decreased admissions
from the ED when albuterol rather than epinephrine is used, neither the meta-analysis
nor another RCT were needed. Contrary to the committee’s assertions, the data show
progressively decreasing admissions from the ED when nebulized normal saline, epinephrine,
or albuterol are used in treatment.
The second rationale relied on by the committee to recommend against the use of albuterol
is a meta-analysis contained in a Cochrane review performed by Gadomski et al. This
meta-analysis reported an OR 0.77, (95% CI [0.44–1.33]) for hospital admission from
the ED.2 This null result was interpreted by the guideline authors as ‘clearly negative.’1,9
Such an interpretation is unfortunate: the statistical power of this analysis to detect
a relative decrease of 20% in admission was 18% (n=404 with the reported sample characteristics,
α=0.05). A null result in an inadequately powered study is no basis for concluding
a drug has no effect.
The committee attached particular weight to placebo-controlled studies, which it regards
as ‘the highest form of evidence,’ and therefore excluded studies that compared bronchodilators
from their deliberations. However, when placebo is not the standard of care then placebo
is not necessarily the best or even correct comparator.10 To demonstrate this effect
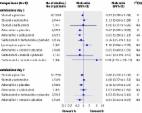
we have recreated the meta-analysis relied on by the committee, this time including
the largest excluded study which did show a benefit to using albuterol in the ED.
(We conservatively assumed epinephrine to be no more effective than placebo, and used
relative risk rather than odds ratios because hospital admission is not rare and risk
is easier to interpret.) The result (Figure) shows that albuterol treatment of bronchiolitis
in the ED leads to decreased admissions and how little underpowered studies contribute
to our knowledge.
We disagree with both components of the committee’s third rationale for not using
bronchodilators. First, the assertion that albuterol non-responders cannot be distinguished
from responders is inaccurate. A therapeutic trial distinguishes them handily. Second,
the committee’s assertion that clinicians are unable to adequately observe clinically
relevant responses to bronchodilators ignores the reality that emergency physicians
are highly experienced in the management of bronchospasm and the use of bronchodilators.
The recommendation that albuterol be withheld from everyone with bronchiolitis because
it may prevent admission in only a minority,1,9 denies clinicians the common sense
practice of the therapeutic trial. If the child responds to albuterol it can be continued;
if not, it can be discontinued.
We also disagree with the committee’s fourth rationale for recommending against the
use of bronchodilators, namely their assessment of the dangers and expense of albuterol.1
Albuterol in reasonable doses has a long record of safety in infants and children;
we even allow primary school children to carry and self-administer it. And premixed
albuterol ampoules retail for 36 cents/dose at a large multipurpose national retailer.
The 18% relative reduction in hospital admissions from the ED that can be obtained
using albuterol is surely also an important part of any cost-benefit calculation.8
Other studies, including a Cochrane review meta-analysis cited by the committee as
evidence against using albuterol, in fact demonstrate that albuterol in the ED significantly
improves clinical scores.2 Clinical scores reflect respiratory distress, which certainly
seems worth relieving. Not all cases of this short-term relief of respiratory distress
will translate into decreased hospital admissions. But some will. This evidence has
been ignored in formulating the current guidelines.1
The second recommendation which emergency physicians might best ignore is that clinicians
may withhold supplemental oxygen if the oxygen saturation is ≥90% rather than the
92% used elsewhere. The committee writing the guidelines base this recommendation
on ‘low level evidence and reasoning from first principles.’1 The committee’s rationale
is that:
Oxygen saturations of 90% are not materially different from oxygen saturations of
92%.
The Collaborative Home Infant Monitoring Evaluation (CHIME) study found that oxygen
desaturations commonly occur in the sleep of normal infants without ill effect.11
This recommendation appears to discount the fact that the normal range of oxygen saturation
for this age group at sea level is 97%–100%.12 It also ignores evidence that a pulse
oximeter reading of 90% tends to overestimate the actual oxygen saturation in children
(mean bias 4.2% between 86% and 90% and 1.8% between 91%–95%).13
There is uncertainty as to what level and duration of hypoxia is harmful in infants
in general and bronchiolitis in particular. Increasing altitude increases the odds
of being at risk for neurodevelopmental problems (100-meter increase in altitude:
OR= 1.02; 95% CI [1.001–1.037] after adjustment for other factors).14 A detailed systematic
review of the literature on hypoxia in children found causal evidence for adverse
effects of chronic and intermittent (as can occur in snoring/sleep disorders) hypoxia
in children. These adverse effects included decreased intelligence quotient (IQ),
neurocognitive functioning, and increases in behavioral disorders and attention deficit
hyperactivity disorder symptoms when oxygen saturation even intermittently ranges
from 90%–94%. These associations are insufficient to prove causality, but these same
adverse effects were also found for hypoxia related to asthma and respiratory instability
in infants.15
The CHIME study found transient oxygen desaturation during sleep is not uncommon in
infants and appears to have little adverse effect.7 However these transient oxygen
desaturations were short: ≤6 seconds duration. When hypoxia occurs in bronchiolitis
it can be expected to be present for hours or days, not seconds. The CHIME study is
simply not pertinent.
Knowing that even relatively mild hypoxia (90%–94%) may have long-term sequelae in
infants, and knowing that the duration of hypoxia of acute bronchiolitis is likely
to be to be prolonged, it is difficult to justify withholding oxygen. Sensible oxygen
administration that avoids hyperoxia is not risky. Whether one should choose an oxygen
saturation treatment threshold of 92% or 94% in previously healthy infants is worthy
of discussion; 90% is probably too low. Studies of neurocognitive function in at least
some infants with treated and untreated hypoxia from bronchiolitis have not been carried
out nor are they likely to be. Waiting for such studies as the committee appears to
be doing strikes us as unwise. However, we can anticipate that in infants, many of
whom will be less than four months old and may still have fetal hemoglobin, the low
Pa02 associated with an Sa02 of 90% will fall yet further after discharge.
These recommendations within the guidelines seem to be premised on an underlying belief
that because bronchiolitis is a short-lived generally non-fatal disease, treatment
cannot offer long-term benefit, and that most treatment should therefore be avoided.
Emergency physicians’ raison d’être however is to treat acute conditions; relieving
acute respiratory distress and hypoxia using interventions as simple as albuterol
and oxygen is not only good emergency medicine practice; it is in fact supported by
the available evidence.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Epinephrine and dexamethasone in children with bronchiolitis.
, Serge Gouin, Natasha Wiebe … (2009)
- Record: found
- Abstract: found
- Article: found
Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis
Lisa Hartling, Ricardo Fernandes, Liza Bialy … (2011)