- Record: found
- Abstract: found
- Article: found
Epidemiology and Natural History of Primary Biliary Cholangitis in the Chinese: A Territory-Based Study in Hong Kong between 2000 and 2015
Read this article at
Abstract
Objectives:
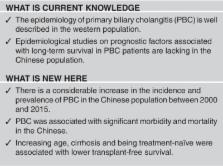
Studies on the epidemiology of primary biliary cholangitis (PBC) in the Chinese population are lacking. We aimed to determine the epidemiology of PBC in Hong Kong (HK) with a population of 7.3 million.
Methods:
We retrieved data from the electronic database of the HK Hospital Authority, the only public healthcare provider in Hong Kong. PBC cases between 2000 and 2015 were identified by International Classification of Diseases (ICD)-9 code. We estimated the age-/sex-adjusted incidence rate and prevalence of PBC, and analyzed the adverse outcomes (hepatocellular carcinoma (HCC), liver transplantation, and death).
Results:
One thousand and sixteen PBC patients aged ≥20 years were identified (female-to-male ratio 4:1; median age 60.6 years, interquartile range (IQR) 51.8–72.6 years; median follow-up 5.6 years, IQR 1.6–8.7 years). The average age/sex-adjusted annual incidence rate and prevalence were 8.4 per million person-years and 56.4 per million, respectively. Between 2000 and 2015, the age/sex-adjusted annual incidence rate increased from 6.7 to 8.1 per million person-years (Poisson P=0.002), while age/sex-adjusted prevalence increased from 31.1 to 82.3 per million (Poisson P<0.001). Fifty patients developed HCC, and 49 underwent liver transplantation. Case fatality risk decreased from 10.8 to 6.4% (Poisson P=0.003). The 5- and 10-year overall survival rates were 81.5 and 78.3%, whereas the transplant-free survival rates were 78.0% and 74.3%, respectively. Increasing age, cirrhosis and being treatment-naïve were associated with lower transplant-free survival.
Related collections
Most cited references14
- Record: found
- Abstract: not found
- Article: not found
Primary biliary cirrhosis.
- Record: found
- Abstract: found
- Article: not found
Primary biliary cirrhosis.
- Record: found
- Abstract: found
- Article: not found