- Record: found
- Abstract: found
- Article: found
COPD from an everyday primary care point of view
Read this article at
Abstract
Introduction:
The purpose of this study is to use real world evidence on treatment use to evaluate drug superiority within the same treatment group.
Methods:
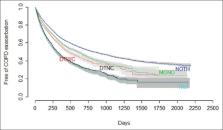
Retrospective cohort analysis using the Spanish Database for Pharmacoepidemiological Research in Primary Care (BIFAP). Data includes longitudinal routine clinical data extracted from practice records of 7,890,485 patients. All subjects with an incident diagnosis of COPD in the database BIFAP between January 1 2010 and December 31 2012 were included in the cohort study. Cox regression analysis was performed to compare the hazard of COPD exacerbation outcome of the four principal cohorts (no therapy, monotherapy, double therapies with and without corticoids, and triple therapy) and within each principal cohort between the different treatment combinations.
Results:
27,739 patients with COPD were included in the analysis. The median age was 64 years, male proportion was 69% and 70% were smokers. 58,042.9 person--years of follow-up were obtained for the cohort with a mean follow-up of 2.09 years per subject. The strongest factor associated with an increased risk of exacerbation was suffering an exacerbation the previous year (HR = 1.82[1.76--1.87 95%CI]). No differences were found between the most frequent monotherapies, double therapies without corticoid, or triple therapy. When comparing the different combinations of double therapies with corticoid, salmeterol/fluticasone combination (HR = 1.16[1.08--1.24]) revealed a higher adjusted hazard of exacerbation when compared with formoterol/budesonide.
Conclusions:
Treatment with a combination of budesonide/formoterol was associated with lower exacerbations than the treatment with fluticasone/salmeterol. The analysis did not reveal any differences in terms of exacerbation in monotherapy, double therapy without corticoids, and triple therapy combinations.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group study.
- Record: found
- Abstract: found
- Article: not found
Comparative Efficacy of Once-Daily Umeclidinium/Vilanterol and Tiotropium/Olodaterol Therapy in Symptomatic Chronic Obstructive Pulmonary Disease: A Randomized Study
- Record: found
- Abstract: found
- Article: not found