- Record: found
- Abstract: found
- Article: found
Effects of Platelet-Rich Plasma on Kidney Regeneration in Gentamicin-Induced Nephrotoxicity
Read this article at
Abstract
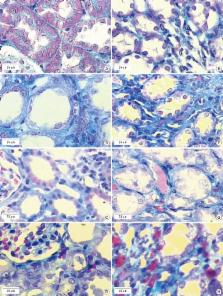
Platelet-rich plasma (PRP) as a source of growth factors may induce tissue repairing and improve fibrosis. This study aimed to assess the effects of PRP on kidney regeneration and fibrosis in gentamicin (GM)-induced nephrotoxicity rat model by stereological study. Thirty-two male rats were selected. Nephrotoxicity was induced in animals by administration of GM (80 mg/kg/daily, intraperitoneally [IP], 8 day) and animals were treated by PRP (100 µL, intra-cortical injection using surgical microscopy, single dose). Blood samples were collected for determine blood urea nitrogen (BUN) and creatinine (Cr) before and after PRP therapy. At the end of experiment, right kidneys were sectioned by Isotropic Uniform Random (IUR) method and stained with H & E and Masson’s Trichrome. The stereological methods were used for estimating the changes in different structures of kidney. PRP increased the number of epithelial cells in convoluted tubules, and decreased the volume of connective tissue, renal corpuscles and glomeruli in GM-treated animals ( P < 0.05). Our findings indicate that PRP had beneficial effects on proliferation of epithelial cells in convoluted tubules and ameliorated GM-induced fibrosis.
Graphical Abstract

Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
The role of growth factors in cartilage repair.
- Record: found
- Abstract: found
- Article: not found