- Record: found
- Abstract: found
- Article: found
Quantification of left ventricular trabeculae using cardiovascular magnetic resonance for the diagnosis of left ventricular non-compaction: evaluation of trabecular volume and refined semi-quantitative criteria
Read this article at
Abstract
Background
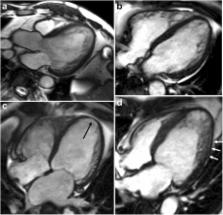
Left ventricular non-compaction (LVNC) is an unclassified cardiomyopathy and there is no consensus on the diagnosis of LVNC. The aims of this study were to establish quantitative methods to diagnose LVNC using cardiovascular magnetic resonance (CMR) and to suggest refined semi-quantitative methods to diagnose LVNC.
Methods
This retrospective study included 145 subjects with mild to severe trabeculation of the left ventricle myocardium [24 patients with isolated LVNC, 33 patients with non-isolated LVNC, 30 patients with dilated cardiomyopathy (DCM) with non-compaction (DCMNC), 27 patients with DCM, and 31 healthy control subjects with mild trabeculation]. The left ventricular (LV) ejection fraction, global LV myocardial volume, trabeculated LV myocardial volume, and number of segments with late gadolinium enhancement were measured. In addition, the most prominent non-compacted (NC), compacted (C), normal mid-septum, normal mid-lateral wall, and apical trabeculation thicknesses on the end-diastolic frames of the long-axis slices were measured.
Results
In the patients with isolated LVNC, the percentage of trabeculated LV volume (TV%, 42.6 ± 13.8 %) relative to total LV myocardial volume was 1.4 times higher than in those with DCM (30.3 ± 14.3 %, p < 0.001), and 1.7 times higher than in the controls (24.8 ± 7.1 %, p < 0.001). However, there was no significant difference in TV% between the isolated LVNC and DCMNC groups (47.1 ± 17.3 % in the DCMNC group; p = 0.210). The receiver operating characteristic curve analysis using Jenni’s method for CMR classification as the standard diagnostic criteria revealed that a value of TV% above 34.6 % was predictive of NC with a specificity of 89.7 % (CI: 74.2 - 98.0 %) and a sensitivity of 66.1 % (CI: 52.6 - 77.9 %). A value of NC/septum over 1.27 was considered predictive for NC with a specificity of 82.8 % (CI: 64.2 - 94.2 %) and a sensitivity of 57.6 % (CI: 44.1 - 70.4 %). In addition, a value of apex/C above 3.15 was considered predictive of NC with a specificity of 93.1 % (CI: 77.2 - 99.2 %) and a sensitivity of 69.5 % (CI: 56.1 - 80.8 %).
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Measuring agreement in method comparison studies.
- Record: found
- Abstract: found
- Article: not found
Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy.
- Record: found
- Abstract: found
- Article: not found