- Record: found
- Abstract: found
- Article: found
The prevalence of benzodiazepines utilization and its association with falls among Saudi older adults; results from the Saudi national survey for elderly Health (SNSEH)
Read this article at
Abstract
Purpose
First, to determine benzodiazepines prevalence (BDZs) among Saudi older adults (SOA); Second, to quantify the association between BDZs use and falls among SOA. Third, to determine falls effect on all-cause mortality among SOA.
Methods
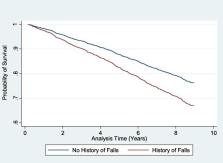
This is a cross-sectional study that used the Saudi National Survey for Elderly Health; a nationally-representative, population-based survey. Participants were asked about BDZs use and falls history during the 12 months prior to the interview. Demographics, medications, comorbidities and housing conditions were used as covariates. Multiple imputation was used to impute missing data. Modified poisson multivariable regression was used to study the association between BDZs and falls. Cox- proportional hazard regression was used to determine falls effect on mortality over nine years period.
Results
Among 2946 SOA, BDZs prevalence was 4%. Around 13% reported falls. In the multivariable regression, relative risk (RR) of falls was 2 comparing BDZs users to non-users (95CI%: 1.02–3.99). Antidepressants (RR = 1.72; 95%CI: 1.10–2.74), laxatives (RR = 1.38; 95%CI: 1.11–1.7), low body mass index (RR = 1.94; 95%CI: 1.33–2.84), mild cognitive impairment (RR = 1.56; 95%CI: 1.21–2.03), high door steps (RR = 1.54; 95%CI: 1.23–1.93) and insufficient illumination (RR = 1.38; 95%CI: 1.11–1.71) increased falls risk. Lastly, the hazard ratio of falls on death was 1.48 (95%CI: 1.17, 1.89) over nine years.
Conclusion
Despite the recommendation against BDZs use among older adults, still there were subjects who were prescribed these drugs. falls are common among SOA. Preventive strategies such medication therapy management, nutrition improvement, elderly-friendly housing structures can reduce the prevalence of falls and consequent increase in mortality among SOA.
Related collections
Most cited references50
- Record: found
- Abstract: found
- Article: not found
Risk factors for falls among elderly persons living in the community.
- Record: found
- Abstract: found
- Article: not found
Meta-analysis of the impact of 9 medication classes on falls in elderly persons.

- Record: found
- Abstract: found
- Article: found