- Record: found
- Abstract: found
- Article: found
Automated immature granulocyte count in patients of the intensive care unit with suspected infection Translated title: Contagem automatizada de granulócitos imaturos em pacientes de uma unidade de terapia intensiva com suspeita de infecção
Read this article at
Abstract
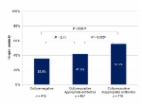
ABSTRACT Introduction: Diagnosing infections in intensive care unit (ICU) patients is vital to provide appropriate therapies. Hematological analyzers perform automated immature granulocyte counts (IG) quickly and with no additional cost when compared to traditional microbiological cultures. Elevated IG is directly associated with infections and inflammation. Objectives: Evaluate IG as infection marker in adult inpatients at the ICU-Complexo Hospital de Clínicas da Universidade Federal do Paraná (CHC-UFPR), compared to cultures of biological materials (gold standard). Material And Methods: Samples of 200 adult inpatients at CHC-UFPR ICU with suspected infection were used. Absolute (IG#) and relative (IG%) counts were performed on the Sysmex XN-3000. Cultures and blood cultures were performed either manually or on Bactec FX. Diagnostic accuracy and agreement for IG# and IG% were evaluated. Results: The reference intervals (RI) obtained for IG# and IG% were 0.06 × 103/µl and 0.6%, respectively, with sensitivity for both of 74.4% and specificity of 25.3% for IG#, and 26.6% for IG%. The receiver operating characteristic (ROC) curve showed cut-off value of 0.33 × 103/µl for IG#, sensitivity of 28%, specificity of 82.3%, and area under the curve (AUC) of 0.521. For IG%, cut-off value was 1.35%, sensitivity 44.6%, specificity 64.6%, and AUC 0.532. CV < 3% increased specificity to 88%. Conclusion: RI of IG% and IG# showed high sensitivity and are useful in screening for infection in ICU patients. The CVs demonstrated by the ROC curves showed high specificity and are helpful on the exclusion of sepsis diagnosis in ICU patients. IG was shown to be useful for screening and confirmation of infection in ICU patients.
Translated abstract
RESUMEN Introducción: Diagnosticar infecciones en pacientes de la unidad de cuidados intensivos (UCI) es de suma importancia para proporcionar el tratamiento adecuado. El contaje automatizado de granulocitos inmaduros (GI) en analizadores hematológicos es rápido y sin costes adicionales. La elevada tasa de GI está asociada a infecciones. Objetivos: Evaluar GI como indicador de infección en pacientes adultos de la UCI del Complexo Hospital de Clínicas da Universidade Federal do Paraná (CHC-UFPR) en comparación a culturas de materiales biológicos (estándar de oro). Material Y Métodos: Se analizaron muestras de 200 pacientes adultos con sospecha de infección de la UCI del CHC-UFPR. Los conteos automatizados de granulocitos inmaduros absolutos (GI#) e relativos (GI%) se realizaron en el Sysmex-XN-3000, y los cultivos y hemocultivos, manualmente o en el Baetec-FX. Se han evaluado precisión diagnóstica y concordancia para GI# y GI%. Resultados: Los rangos de referencia obtenidos para GI# y GI% fueron 0,06 × 103/µl y 0,6%, respectivamente, con sensibilidad para ambos de 74,4% y especificidad de 25,3% para IG# y 26,6% para IG%. La curva receiver operating characteristic (ROC) ha mostrado valor de corte de 0,33 × 103/µl para IG#, sensibilidad de 28%, especificidad de 82,3% y área bajo la curva (AUC) de 0,521. Para GI%, el valor de corte ha sido 135%, sensibilidad de 44,6%, especificidad de 64,6% y AUC de 0,532. Valores de corte de GI% < 3% aumentaron la especificidad para 88%. Conclusión: Rangos de referencia de GI% y GI# presentaron sensibilidad elevada y son útiles en el triaje de infecciones en pacientes de UCI. Los valores de corte enseñados por las curvas ROC presentaron alta especificidad, permitiendo la identificación adecuada de los pacientes sanos. GI se ha mostrado útil para triaje y confirmación de infección en pacientes de UCI.
Translated abstract
RESUMO Introdução: Diagnosticar infecções em pacientes da unidade de terapia intensiva (UTI) é vital para implementar terapias apropriadas. A contagem automatizada de granulócitos imaturos (IG) em analisadores hematológicos é rápida e sem custos adicionais. A taxa de IG elevada está associada a infecções. Objetivos: Avaliar IG como indicador de infecção em pacientes adultos da UTI do Complexo Hospital de Clínicas da Universidade Federal do Paraná (CHC-UFPR) em comparação com culturas de materiais biológicos (padrão-ouro). Material E Métodos: Foram analisadas amostras de 200 pacientes adultos com suspeita de infecção da UTI do CHC-UFPR. As contagens automatizadas de granulócitos imaturos absolutas (IG#) e relativas (IG%) foram realizadas no Sysmex-XN-3000, e as culturas e as hemoculturas, manualmente ou no Bactec-FX. As características de desempenho de teste diagnóstico para IG# e IG% foram avaliadas. Resultados: Os intervalos de referência (IR) obtidos para IG# e IG% foram 0,06 × 103/µl e 0,6%, respectivamente, com sensibilidade para ambos de 74,4% e especificidade de 25,3% para IG# e 26,6% para IG%. A curva receiver operating characteristic (ROC) mostrou valor de corte de 0,33 × 103/µl para IG#, sensibilidade de 28%, especificidade de 82,3% e área sob a curva (AUC) de 0,521. Para IG%, o valor de corte foi de 1,35%, sensibilidade de 44,6%, especificidade de 64,6% e AUC de 0,532. Valores de corte de IG% < 3% aumentaram a especificidade para 88%. Conclusão: IRs de IG% e IG# apresentaram sensibilidade elevada e são úteis na triagem de infecção nos pacientes da UTI. Os VCs demonstrados pelas curvas ROC para IG% e IG# apresentaram elevada especificidade, sendo, portanto, úteis para exclusão de diagnóstico de sepse nos pacientes da UTI. IG mostrou-se útil para triagem e confirmação de infecção em pacientes de UTI.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
A Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2013 Recommendations by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM) a
- Record: found
- Abstract: not found
- Article: not found
The epidemiology of sepsis in Brazilian intensive care units (the Sepsis PREvalence Assessment Database, SPREAD): an observational study
- Record: found
- Abstract: found
- Article: found