- Record: found
- Abstract: found
- Article: found
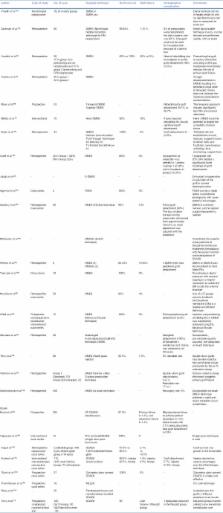
Component corneal surgery: An update
Read this article at
Abstract
Several decades ago, penetrating keratoplasty was a challenge to corneal surgeons. Constant effort by the corneal surgeon to improve the outcomes as well as utilization of the available resources has led to a revolutionary change in the field of keratoplasty. All these efforts have led to the evolution of techniques that allow a corneal surgeon to disease-specific transplant of individual layers of corneal “so-called component corneal surgery” depending on the layer of cornea affected. This has led to an improvement in corneal graft survival as well as a better utilization of corneal tissues. This article reviews the currently available literature on component corneal surgeries and provides an update on the available techniques.
Related collections
Most cited references98
- Record: found
- Abstract: found
- Article: not found
Descemet membrane endothelial keratoplasty (DMEK).
- Record: found
- Abstract: found
- Article: not found
Preliminary clinical results of Descemet membrane endothelial keratoplasty.
- Record: found
- Abstract: found
- Article: not found