- Record: found
- Abstract: found
- Article: found
Burden of disease in francophone Africa, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017
Read this article at
Summary
Background
Peer-reviewed literature on health is almost exclusively published in English, limiting the uptake of research for decision making in francophone African countries. We used results from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017 to assess the burden of disease in francophone Africa and inform health professionals and their partners in the region.
Methods
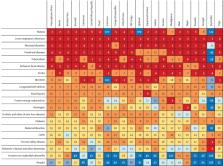
We assessed the burden of disease in the 21 francophone African countries and compared the results with those for their non-francophone counterparts in three economic communities: the Economic Community of West African States, the Economic Community of Central African States, and the Southern African Development Community. GBD 2017 employed a variety of statistical models to determine the number of deaths from each cause, through the Cause of Death Ensemble model algorithm, using CoDCorrect to ensure that the number of deaths per cause did not exceed the total number of estimated deaths. After producing estimates for the number of deaths from each of the 282 fatal outcomes included in the GBD 2017 list of causes, the years of life lost (YLLs) due to premature death were calculated. Years lived with disability (YLDs) were estimated as the product of prevalence and a disability weight for all mutually exclusive sequelae. Disability-adjusted life-years (DALYs) were calculated as the sum of YLLs and YLDs. All calculations are presented with 95% uncertainty intervals (UIs). A sample of 1000 draws was taken from the posterior distribution of each estimation step; aggregation of uncertainty across age, sex, and location was done on each draw, assuming independence of uncertainty. The lower and upper UIs represent the ordinal 25th and 975th draws of each quantity and attempt to describe modelling as well as sampling error.
Findings
In 2017, 779 deaths (95% UI 750–809) per 100 000 population occurred in francophone Africa, a decrease of 45·3% since 1990. Malaria, lower respiratory infections, neonatal disorders, diarrhoeal diseases, and tuberculosis were the top five Level 3 causes of death. These five causes were found among the six leading causes of death in most francophone countries. In 2017, francophone Africa experienced 53 570 DALYs (50 164–57 361) per 100 000 population, distributed between 43 708 YLLs (41 673–45 742) and 9862 YLDs (7331–12 749) per 100 000 population. In 2017, YLLs constituted the majority of DALYs in the 21 countries of francophone Africa. Age-specific and cause-specific mortality and population ageing were responsible for most of the reductions in disease burden, whereas population growth was responsible for most of the increases.
Interpretation
Francophone Africa still carries a high burden of communicable and neonatal diseases, probably due to the weakness of health-care systems and services, as evidenced by the almost complete attribution of DALYs to YLLs. To cope with this burden of disease, francophone Africa should define its priorities and invest more resources in health-system strengthening and in the quality and quantity of health-care services, especially in rural and remote areas. The region could also be prioritised in terms of technical and financial assistance focused on achieving these goals, as much as on demographic investments including education and family planning.
Related collections
Most cited references17
- Record: found
- Abstract: not found
- Article: not found
GBD 2010: design, definitions, and metrics.

