- Record: found
- Abstract: found
- Article: found
Reducing stigma among healthcare providers to improve mental health services (RESHAPE): protocol for a pilot cluster randomized controlled trial of a stigma reduction intervention for training primary healthcare workers in Nepal
Read this article at
Abstract
Background
Non-specialist healthcare providers, including primary and community healthcare workers, in low- and middle-income countries can effectively treat mental illness. However, scaling-up mental health services within existing health systems has been limited by barriers such as stigma against people with mental illness. Therefore, interventions are needed to address attitudes and behaviors among non-specialists. Aimed at addressing this gap, REducing Stigma among Healthc Are Providers to Improv E mental health services (RESHAPE) is an intervention in which social contact with mental health service users is added to training for non-specialist healthcare workers integrating mental health services into primary healthcare.
Methods
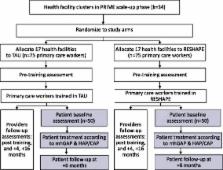
This protocol describes a mixed methods pilot and feasibility study in primary care centers in Chitwan, Nepal. The qualitative component will include key informant interviews and focus group discussions. The quantitative component consists of a pilot cluster randomized controlled trial (c-RCT), which will establish parameters for a future effectiveness study of RESHAPE compared to training as usual (TAU). Primary healthcare facilities (the cluster unit, k = 34) will be randomized to TAU or RESHAPE. The direct beneficiaries of the intervention are the primary healthcare workers in the facilities ( n = 150); indirect beneficiaries are their patients ( n = 100). The TAU condition is existing mental health training and supervision for primary healthcare workers delivered through the Programme for Improving Mental healthcarE (PRIME) implementing the mental health Gap Action Programme (mhGAP). The primary objective is to evaluate acceptability and feasibility through qualitative interviews with primary healthcare workers, trainers, and mental health service users. The secondary objective is to collect quantitative information on health worker outcomes including mental health stigma (Social Distance Scale), clinical knowledge (mhGAP), clinical competency (ENhancing Assessment of Common Therapeutic factors, ENACT), and implicit attitudes (Implicit Association Test, IAT), and patient outcomes including stigma-related barriers to care, daily functioning, and symptoms.
Discussion
The pilot and feasibility study will contribute to refining recommendations for implementation of mhGAP and other mental health services in primary healthcare settings in low-resource health systems. The pilot c-RCT findings will inform an effectiveness trial of RESHAPE to advance the evidence-base for optimal approaches to training and supervision for non-specialist providers.
Related collections
Most cited references71
- Record: found
- Abstract: not found
- Article: not found
Enabling the implementation of evidence based practice: a conceptual framework

- Record: found
- Abstract: found
- Article: found
Individual determinants of research utilization by nurses: a systematic review update
- Record: found
- Abstract: found
- Article: not found