- Record: found
- Abstract: found
- Article: found
Elevated HDL Levels Linked to Poorer Cognitive Ability in Females With Parkinson’s Disease
Read this article at
Abstract
Introduction
Cholesterol levels have been associated with age-related cognitive decline, however, such an association has not been comprehensively explored in people with Parkinson’s disease (PD). To address this uncertainty, the current cross-sectional study examined the cholesterol profile and cognitive performance in a cohort of PD patients.
Methods
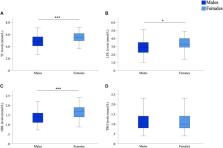
Cognitive function was evaluated using two validated assessments (ACE-R and SCOPA-COG) in 182 people with PD from the Australian Parkinson’s Disease Registry. Total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and Triglyceride (TRG) levels were examined within this cohort. The influence of individual lipid subfractions on domain-specific cognitive performance was investigated using covariate-adjusted generalised linear models.
Results
Females with PD exhibited significantly higher lipid subfraction levels (TC, HDL, and LDL) when compared to male counterparts. While accounting for covariates, HDL levels were strongly associated with poorer performance across multiple cognitive domains in females but not males. Conversely, TC and LDL levels were not associated with cognitive status in people with PD.
Related collections
Most cited references96
- Record: found
- Abstract: found
- Article: not found
Systematic review of levodopa dose equivalency reporting in Parkinson's disease.
- Record: found
- Abstract: found
- Article: not found
Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials
- Record: found
- Abstract: not found
- Article: not found