- Record: found
- Abstract: found
- Article: found
Drop in lung function during asthma and COPD exacerbations – can it be assessed without spirometry?
Abstract
Background
When assessing patients with exacerbation of asthma or COPD, it may be useful to know the drop in forced expiratory volume in 1 second (FEV 1) compared with stable state, in particular when considering treatment with oral corticosteroids. The objective of the study was to identify indicators of drop in FEV 1 during exacerbations.
Methods
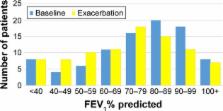
In this prospective multicenter study from primary care, patients diagnosed with asthma or COPD were examined at stable state and during exacerbations the following year. Symptoms, chest findings, and pulse oximetry were recorded, and spirometry was performed. A fixed drop in FEV 1 (10% and ≥200 mL) and percentage change in FEV 1 were outcomes when possible indicators were evaluated.
Results
Three hundred and eighty patients attended baseline examination, and 88 with a subsequent exacerbation were included in the analysis. Thirty (34%) had a significant drop in FEV 1 (10% and 200 mL). Increased wheezing was the only symptom associated with this drop with a likelihood ratio of 6.4 (95% confidence interval, 1.9–21.7). Crackles and any new auscultation finding were also associated with a significant drop in FEV 1, as was a ≥2% drop in oxygen saturation (SpO 2) to ≤92% in the subgroup diagnosed with COPD. Very bothersome wheezing and severe decrease in SpO 2 were also very strong predictors of change in FEV 1 in linear regression adjusted for age, gender, and baseline FEV 1% predicted.
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Susceptibility to exacerbation in chronic obstructive pulmonary disease.
- Record: found
- Abstract: found
- Article: not found
Recent asthma exacerbations: a key predictor of future exacerbations.

- Record: found
- Abstract: found
- Article: found