- Record: found
- Abstract: found
- Article: found
Quality of Care for Acute Kidney Disease: Current Knowledge Gaps and Future Directions
Read this article at
Abstract
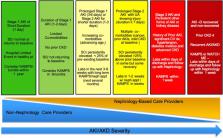
Acute kidney injury (AKI) and acute kidney disease (AKD) are common complications in hospitalized patients and are associated with adverse outcomes. Although consensus guidelines have improved the care of patients with AKI and AKD, guidance regarding quality metrics in the care of patients after an episode of AKI or AKD is limited. For example, few patients receive follow-up laboratory testing of kidney function or post-AKI or AKD care through nephrology or other providers. Recently, the Acute Disease Quality Initiative developed a consensus statement regarding quality improvement goals for patients with AKI or AKD specifically highlighting efforts regarding quality and safety of care after hospital discharge after an episode of AKI or AKD. The goal is to use these measures to identify opportunities for improvement that will positively affect outcomes. We recommend that health care systems quantitate the proportion of patients who need and actually receive follow-up care after the index AKI or AKD hospitalization. The intensity and appropriateness of follow-up care should depend on patient characteristics, severity, duration, and course of AKI of AKD, and should evolve as evidence-based guidelines emerge. Quality indicators for discharged patients with dialysis requiring AKI or AKD should be distinct from end-stage renal disease measures. Besides, there should be specific quality indicators for those still requiring dialysis in the outpatient setting after AKI or AKD. Given the limited preexisting data guiding the care of patients after an episode of AKI or AKD, there is ample opportunity to establish quality measures and potentially improve patient care and outcomes. This review will provide specific evidence-based and expert opinion–based guidance for the care of patients with AKI or AKD after hospital discharge.
Related collections
Most cited references53
- Record: found
- Abstract: found
- Article: found
KDIGO Clinical Practice Guidelines for Acute Kidney Injury
- Record: found
- Abstract: found
- Article: not found
Acute kidney injury, mortality, length of stay, and costs in hospitalized patients.
- Record: found
- Abstract: found
- Article: found