- Record: found
- Abstract: found
- Article: found
The impact of topical lidocaine and timing of LMA removal on the incidence of airway events during the recovery period in children: a randomized controlled trial
Read this article at
Abstract
Background
The timing of laryngeal mask airway (LMA) removal remains undefined. This study aimed to assess the optimal timing for LMA removal and whether topical anesthesia with lidocaine could reduce airway adverse events.
Methods
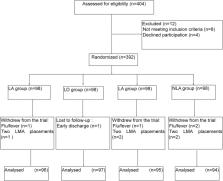
This randomized controlled trial assessed one-to-six-year-old children with ASA I-II scheduled for squint correction surgery under general anesthesia. The children were randomized into the LA (lidocaine cream smeared to the cuff of the LMA before insertion, with mask removal in the awake state), LD (lidocaine application and LMA removal under deep anesthesia), NLA (hydrosoluble lubricant application and LMA removal in the awake state) and NLD (hydrosoluble lubricant application and LMA removal in deep anesthesia) groups. The primary endpoint was a composite of irritating cough, laryngeal spasm, SpO 2 < 96%, and glossocoma in the recovery period in the PACU. The secondary endpoints included the incidence of pharyngalgia and hoarseness within 24 h after the operation, duration of PACU stay, and incidence of agitation in the recovery period. The assessor was unblinded.
Results
Each group included 98 children. The overall incidence of adverse airway events was significantly lower in the LA group (9.4%) compared with the LD (23.7%), NLA (32.6%), and NLD (28.7%) groups ( P=0.001). Cough and laryngeal spasm rates were significantly higher in the NLA group (20.0 and 9.5%, respectively) than the LA (5.2 and 0%, respectively), LD (4.1 and 1.0%, respectively), and NLD (9.6 and 2.1%, respectively) groups ( P=0.001). Glossocoma incidence was significantly lower in the LA and NLA groups (0%) than in the LD (19.6%) and NLD (20.2%) groups ( P< 0.001). At 24 h post-operation, pharyngalgia incidence was significantly higher in the NLA group (15.8%) than the LA (3.1%), LD (1.0%), and NLD (3.2%) groups ( P< 0.001).
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
Incidence and risk factors of perioperative respiratory adverse events in children undergoing elective surgery.
- Record: found
- Abstract: found
- Article: not found
Risk factors for perioperative adverse respiratory events in children with upper respiratory tract infections.
- Record: found
- Abstract: found
- Article: not found