- Record: found
- Abstract: found
- Article: found
A prospective population-based cohort study of lactation and cardiovascular disease mortality: the HUNT study
Read this article at
Abstract
Background
Recent studies suggest that lactation has long-term effects on risk for cardiovascular disease in women, but the effects on cardiovascular mortality are less well known.
Method
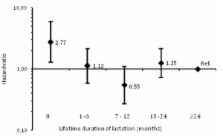
In a Norwegian population-based prospective cohort study, we studied the association of lifetime duration of lactation with cardiovascular mortality in 21,889 women aged 30 to 85 years who attended the second Nord-Trøndelag Health Survey (HUNT2) in 1995–1997. The cohort was followed for mortality through 2010 by a linkage with the Cause of Death Registry. Adjusted hazard ratios (HR) for death from all causes and cardiovascular disease were calculated using Cox regression.
Results
During follow-up, 1,246 women died from cardiovascular disease. Parous women younger than 65 years who had never lactated had a higher cardiovascular mortality than the reference group of women who had lactated 24 months or more (HR 2.77, 95% confidence interval [CI]: 1.28, 5.99). There was some evidence of a U-shaped association, where women who reported lactating 7–12 months had a HR of 0.55 (95% CI: 0.27, 1.09). No clear associations were observed among women 65 years or older.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Duration of lactation and incidence of type 2 diabetes.
- Record: found
- Abstract: found
- Article: found
A systematic review of maternal obesity and breastfeeding intention, initiation and duration

- Record: found
- Abstract: found
- Article: found