- Record: found
- Abstract: found
- Article: found
Electrocardiogram interpretation among pediatricians: Assessing knowledge, attitudes, and practice
Read this article at
Abstract
Objectives:
This study assesses the competency of pediatricians in interpreting electrocardiograms (ECGs).
Methods:
A cross-sectional study involving 125 pediatricians comprised of 71 general pediatricians, 15 pediatric cardiologists, and 39 other subspecialists recruited from all public hospitals and two specialty centers. Participants completed a questionnaire that included 10 ECGs and questions regarding backgrounds, attitudes, and practices. The ECGs were graded to obtain a knowledge score out of 30 points. Mann–Whitney U test and Kruskal-Wallis test with post hoc analysis and Bonferroni adjustment were used to compare groups.
Results:
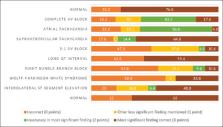
The mean knowledge score ranged from 47.7% to 69.7% among various pediatric specialties ( P = 0.006). Age, increasing years of experience, confidence level, number of cardiology referrals, and perceived importance of having good ECG interpretation skills were significantly related to the knowledge score ( P ≤ 0.05). Accuracy was highest in identifying normal ECGs (76.8%), supraventricular tachycardia (64.8%), along with long QT interval (58.4%), and was lowest for right bundle branch block (RBBB) (10.4%), 2:1 atrioventricular conduction (10.4%), and atrial tachycardia (AT) (4.8%). Accuracy among pediatric cardiologists was highest for long QT interval (100%), normal ECG (80%), as well as Wolff-Parkinson-White syndrome (80%), and lowest for RBBB (13.3%) and AT (0%). Most pediatricians believe that ECGs are “useful” (78.4%) and that having good interpretation skill is “important” (80.6%).
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
Competency in interpretation of 12-lead electrocardiograms: a summary and appraisal of published evidence.

- Record: found
- Abstract: found
- Article: found
Congenital and childhood atrioventricular blocks: pathophysiology and contemporary management
- Record: found
- Abstract: found
- Article: not found