- Record: found
- Abstract: found
- Article: found
“Breathing New Life Into Chronic Obstructive Pulmonary Disease (COPD)” – Results From An Online Survey Of UK Patients
Abstract
Background
There is a lack of data on the impact of COPD on individuals, their illness, behavior and attitude to the disease.
Results
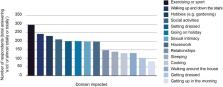
61.2% of respondents were female and 85.8% were between 50 and 80 years old. Two-thirds (67.8%) of respondents did not smoke at the time of the survey. Almost half of those surveyed (46.2%, n=231) used three inhalers, and 31% (n=155) agreed or strongly agreed with the statement “I feel that my treatment is not adequately controlling my condition”, while 39.4% (n=197) disagreed or strongly disagreed. 48.8% (n=244) agreed their COPD was well managed. Over half the sample (56.8%, n=284) said they never forgot to use their inhaler as prescribed. Checks on inhaler use by doctors or nurses were reported as every six months/twice a year by 24.4% (n=122) and once a year by 38.8% (n=194). However, 17.2% (n=86) said their technique had never been checked, and at their last annual review, a third (33.2%, n=166) did not receive inhaler technique advice. Exacerbations were reported to affect an average of 7.4 days a year. They led to time in hospital, time off work and significantly affected quality of life. Patients reported that their COPD affected all aspects of their daily lives to a greater or lesser extent, with some living in fear of what the impact of the next flare-up could bring.
Conclusion
COPD impairs people’s ability to carry out daily tasks, leads to hospital admission, time off work and even unemployment. Respondents reported stress, worry and depression or low mood because of their COPD. This study highlights areas of concern for patients not being addressed by health care practitioners, including: pulmonary rehabilitation referral, better information giving and medicines optimization.
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Susceptibility to exacerbation in chronic obstructive pulmonary disease.

- Record: found
- Abstract: found
- Article: found
Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns
- Record: found
- Abstract: found
- Article: not found