- Record: found
- Abstract: found
- Article: found
High detection rate in [ 18F]PSMA-1007 PET: interim results focusing on biochemical recurrence in prostate cancer patients
Read this article at
Abstract
Objective
18F-labeled prostate-specific membrane antigen (PSMA) ligand, [ 18F]PSMA-1007, has the benefit of a higher synthetic yield and minimal excretion in the urine. High detection efficacy was reported in biochemical recurrence (BCR) of prostate cancer after radical prostatectomy. Thus, we evaluated the preliminary diagnostic utility of [ 18F]PSMA-1007 PET in patients with prostate cancer, focusing on the BCR which is not detected on conventional imaging.
Methods
We enrolled a total of 28 patients (age 51–79 years) with BCR of prostate cancer. BCR was defined as a continuous increase in PSA after radical prostatectomy or radiation therapy without any apparent recurrent lesions on conventional diagnostic imaging (CT and bone scintigraphy). PSMA-PET scanning was performed approximately 60 min after intravenous injection of [ 18F]PSMA-1007 (259 ± 37 MBq). PSMA-PET images were evaluated for lesion detection as well as its relation to PSA values and location.
Results
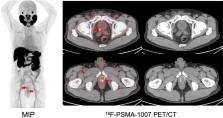
Abnormal uptake, which was suspected to be recurrence or metastasis, was detected in 92.9% (26/28) of patients with BCR. The SUVmax was 8.4 ± 6.4 in local recurrence, 11.5 ± 11.8 in pelvic lymph nodes (LN), and 4.1 ± 1.6 in bone metastasis. The detection rates were 66.7% in the PSA group-1 (0.1–0.5 ng/mL), 85.7% in the PSA group-2 (0.5–1.0 ng/mL), and 100% in the PSA group-3 (above 1.0 ng/mL). Among the PET-positive BCR patients ( n = 26), local recurrence was detected in 57.7% (15/26), pelvic LN in 42.3% (11/26), and bone metastasis in 15.4% (4/26). In 53% (8/15) of BCR patients who were suspected of local recurrence, focal uptake was detected adjacent to the bladder on [ 18F]PSMA-1007 PET. This suggested the significant advantage of having minimal physiological urine excretion.
Related collections
Most cited references13

- Record: found
- Abstract: found
- Article: found
F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients

- Record: found
- Abstract: found
- Article: found
Detection Efficacy of 18 F-PSMA-1007 PET/CT in 251 Patients with Biochemical Recurrence of Prostate Cancer After Radical Prostatectomy
- Record: found
- Abstract: found
- Article: not found