- Record: found
- Abstract: found
- Article: found
Cardiac Resynchronization Therapy and QRS Duration: Systematic Review, Meta-analysis, and Meta-regression

Read this article at
Abstract
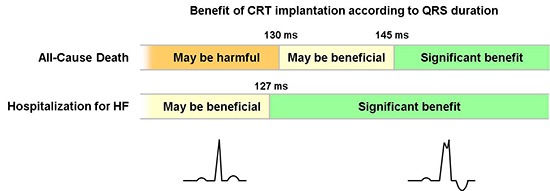
Cardiac resynchronization therapy (CRT) has been shown to reduce the risk of death and hospitalization in patients with advanced heart failure with left ventricular dysfunction. However, controversy remains regarding who would most benefit from CRT. We performed a meta-analysis, and meta-regression in an attempt to identify factors that determine the outcome after CRT. A total of 23 trials comprising 10,103 patients were selected for this meta-analysis. Our analysis revealed that CRT significantly reduced the risk of all-cause mortality and hospitalization for heart failure compared to control treatment. The odds ratio (OR) of all-cause death had a linear relationship with mean QRS duration ( P=0.009). The benefit in survival was confined to patients with a QRS duration ≥145 ms (OR, 0.86; 95% CI, 0.74-0.99), while no benefit was shown among patients with a QRS duration of 130 ms (OR, 1.00; 95% CI, 0.80-1.25) or less. Hospitalization for heart failure was shown to be significantly reduced in patients with a QRS duration ≥127 ms (OR, 0.77; 95% CI, 0.60-0.98). This meta-regression analysis implies that patients with a QRS duration ≥150 ms would most benefit from CRT, and in those with a QRS duration <130 ms CRT implantation may be potentially harmful.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Cardiac-resynchronization therapy for the prevention of heart-failure events.
- Record: found
- Abstract: found
- Article: not found
Cardiac-resynchronization therapy for mild-to-moderate heart failure.
- Record: found
- Abstract: found
- Article: not found