- Record: found
- Abstract: found
- Article: found
A systems-based partnership learning model for strengthening primary healthcare
Read this article at
Abstract
Background
Strengthening primary healthcare systems is vital to improving health outcomes and reducing inequity. However, there are few tools and models available in published literature showing how primary care system strengthening can be achieved on a large scale. Challenges to strengthening primary healthcare (PHC) systems include the dispersion, diversity and relative independence of primary care providers; the scope and complexity of PHC; limited infrastructure available to support population health approaches; and the generally poor and fragmented state of PHC information systems.
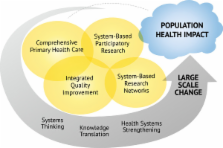
Drawing on concepts of comprehensive PHC, integrated quality improvement (IQI) methods, system-based research networks, and system-based participatory action research, we describe a learning model for strengthening PHC that addresses these challenges. We describe the evolution of this model within the Australian Aboriginal and Torres Strait Islander primary healthcare context, successes and challenges in its application, and key issues for further research.
Discussion
IQI approaches combined with system-based participatory action research and system-based research networks offer potential to support program implementation and ongoing learning across a wide scope of primary healthcare practice and on a large scale. The Partnership Learning Model (PLM) can be seen as an integrated model for large-scale knowledge translation across the scope of priority aspects of PHC. With appropriate engagement of relevant stakeholders, the model may be applicable to a wide range of settings. In IQI, and in the PLM specifically, there is a clear role for research in contributing to refining and evaluating existing tools and processes, and in developing and trialling innovations. Achieving an appropriate balance between funding IQI activity as part of routine service delivery and funding IQI related research will be vital to developing and sustaining this type of PLM.
Summary
This paper draws together several different previously described concepts and extends the understanding of how PHC systems can be strengthened through systematic and partnership-based approaches. We describe a model developed from these concepts and its application in the Australian Indigenous primary healthcare context, and raise questions about sustainability and wider relevance of the model.
Related collections
Most cited references43
- Record: found
- Abstract: not found
- Article: not found
Communities of Practice and Social Learning Systems

- Record: found
- Abstract: found
- Article: found
Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges
- Record: found
- Abstract: found
- Article: not found