- Record: found
- Abstract: found
- Article: found
Hepatorenal syndrome: the 8 th international consensus conference of the Acute Dialysis Quality Initiative (ADQI) Group
Read this article at
Abstract
Introduction
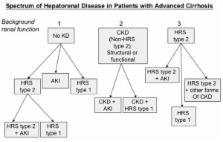
Renal dysfunction is a common complication in patients with end-stage cirrhosis. Since the original publication of the definition and diagnostic criteria for the hepatorenal syndrome (HRS), there have been major advances in our understanding of its pathogenesis. The prognosis of patients with cirrhosis who develop HRS remains poor, with a median survival without liver transplantation of less than six months. However, a number of pharmacological and other therapeutic strategies have now become available which offer the ability to prevent or treat renal dysfunction more effectively in this setting. Accordingly, we sought to review the available evidence, make recommendations and delineate key questions for future studies.
Methods
We undertook a systematic review of the literature using Medline, PubMed and Web of Science, data provided by the Scientific Registry of Transplant Recipients and the bibliographies of key reviews. We determined a list of key questions and convened a two-day consensus conference to develop summary statements via a series of alternating breakout and plenary sessions. In these sessions, we identified supporting evidence and generated recommendations and/or directions for future research.
Results
Of the 30 questions considered, we found inadequate evidence for the majority of questions and our recommendations were mainly based on expert opinion. There was insufficient evidence to grade three questions, but we were able to develop a consensus definition for acute kidney injury in patients with cirrhosis and provide consensus recommendations for future investigations to address key areas of uncertainty.
Conclusions
Despite a paucity of sufficiently powered prospectively randomized trials, we were able to establish an evidence-based appraisal of this field and develop a set of consensus recommendations to standardize care and direct further research for patients with cirrhosis and renal dysfunction.
Related collections
Most cited references131
- Record: found
- Abstract: found
- Article: found
Prediction of Creatinine Clearance from Serum Creatinine
- Record: found
- Abstract: found
- Article: not found
Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study.
- Record: found
- Abstract: found
- Article: not found