- Record: found
- Abstract: found
- Article: found
The safety and efficacy of mycophenolate mofetil in children and adolescents with steroid-dependent nephrotic syndrome: a single-centre study
Read this article at
Abstract
Background
Steroid-dependent nephrotic syndrome (SDNS) patients experience frequent relapse or adverse effects on long-term treatment with steroids or cyclophosphamide. This study assessed the efficacy and side effect profile of mycophenolate mofetil (MMF) therapy in children with nephrotic syndrome in our population.
Methods
A retrospective study was performed on children with SDNS who were on MMF therapy for a minimum period of 1 year, and were on regular follow-up in the Department of Nephrology at the Institute of Child Health and hospital for children attached to Madras Medical College.
Results
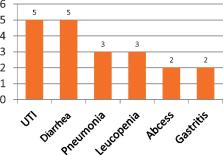
The study included 87 patients, with a male:female ratio of 2:1. The median age at diagnosis of nephrotic syndrome was 3 years [95% confidence interval (CI): 1–8 years], which was found to be a statistically significant risk factor for MMF failure. The median duration of follow-up after initiation of MMF therapy was 3 years and 3 months (95% CI: 1 year and 3 months to 6 years and 6 months). At initial evaluation, 31 (36%) patients presented with SDNS while the remaining had frequently relapsing nephrotic syndrome progressing to SDNS. Intravenous cyclophosphamide was used as first-line therapy in 82 patients, of whom 24 patients had persistent proteinuria while the remaining 58 had attained remission for a median duration of 6 months. The median duration of treatment with MMF was 2 years and 6 months (95% CI: 1 year and 3 months to 4 years and 6 months). MMF was used at a mean dose of 28.5 mg/kg. Seventy-two (83%) patients were MMF-sensitive, and these patients had a reduction in mean prednisolone dose from 1.28 to 0.35 mg/kg (P < 0.05). Among the MMF-sensitive patients, 31 had stopped MMF after a minimum period of 2 years, following which they had a median remission period of 5 months (95% CI: 1–8 months). MMF failure occurred in 15 (17%) patients. Adverse events were documented in 19 (22%) patients.
Related collections
Most cited references11
- Record: found
- Abstract: not found
- Article: not found
Immunosuppressive and other effects of mycophenolic acid and an ester prodrug, mycophenolate mofetil.
- Record: found
- Abstract: found
- Article: not found
A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children.
- Record: found
- Abstract: found
- Article: not found