- Record: found
- Abstract: found
- Article: found
Efficacy and safety of eribulin in patients with locally advanced or metastatic breast cancer not meeting trial eligibility criteria: a retrospective study

Read this article at
Abstract
Background
The efficacy and safety of eribulin in patients with locally advanced or metastatic breast cancer has been demonstrated in phase III trials. However, as patients receiving eribulin in daily practice do not necessarily meet all the eligibility criteria of clinical trials, data for such patients are limited.
Methods
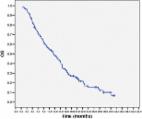
We identified patients with locally advanced or metastatic breast cancer, treated with eribulin monotherapy between July 2011 and December 2015 at the National Cancer Center Hospital, Tokyo, Japan. Patients who would have met the following eligibility criteria from the EMBRACE trial were included in the eligible group, and the rest were included in the ineligible group: 1) Eastern Cooperative Oncology Group Performance status 0–2; 2) adequate function of principal organs; and 3) absence of active infection. We compared the relative dose intensity (RDI), tumor response, progression-free survival (PFS), overall survival (OS), and adverse events between the groups. Nominal and continuous values were compared using the Fisher’s exact test and Mann-Whitney U test, respectively. Survival outcomes were determined using Kaplan-Meier estimation, and between-group differences were assessed using the log-rank test.
Results
Of the 203 patients included, 34 were classified into the ineligible group and 169 into the eligible group. Initial dose reduction and treatment discontinuation due to adverse events (AEs) were more common in the ineligible group (initial dose reduction: 23.5% in the ineligible group vs. 7.7% in the eligible group, p = 0.011; treatment discontinuation due to AEs: 11.8% vs. 3.0%, p = 0.045). However, RDI (66% vs. 71%, p = 0.130), response rate (15.6% vs. 18.1%, p = 1.000), PFS (3.7 months vs. 4.0 months, p = 0.913), OS (11.5 months vs. 16.1 months, p = 0.743), AEs requiring hospitalization (5.9% vs. 6.5%, p = 1.000), and grade 3/4 AEs were similar in both groups. PFS, OS, AEs requiring hospitalization, and discontinuation due to AEs in the eligible group were comparable to those found in previous phase III trials.
Conclusion
The safety and efficacy of eribulin monotherapy was demonstrated in a broader patient population than that eligible for clinical trials. Eribulin may be a treatment option in these patients with locally advanced or metastatic breast cancer, considering dose reduction and pre-existing dysfunctions.
Related collections
Most cited references6

- Record: found
- Abstract: found
- Article: found
Eribulin Mesylate in Pretreated Breast Cancer Patients: A Multicenter Retrospective Observational Study
- Record: found
- Abstract: found
- Article: found
