- Record: found
- Abstract: found
- Article: found
Safety and Efficacy of Ranibizumab in Diabetic Macular Edema (RESOLVE Study*) : A 12-month, randomized, controlled, double-masked, multicenter phase II study
Read this article at
Abstract
OBJECTIVE
The expression of vascular endothelial growth factor (VEGF) is elevated in diabetic macular edema (DME). Ranibizumab binds to and inhibits multiple VEGF variants. We investigated the safety and efficacy of ranibizumab in DME involving the foveal center.
RESEARCH DESIGN AND METHODS
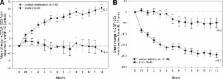
This was a 12-month, multicenter, sham-controlled, double-masked study with eyes (age >18 years, type 1 or 2 diabetes, central retinal thickness [CRT] ≥300 μm, and best corrected visual acuity [BCVA] of 73–39 ETDRS letters [Early Treatment Diabetic Retinopathy Study]) randomly assigned to intravitreal ranibizumab (0.3 or 0.5 mg; n = 51 each) or sham ( n = 49). The treatment schedule comprised three monthly injections, after which treatment could be stopped/reinitiated with an opportunity for rescue laser photocoagulation (protocol-defined criteria). After month 1, dose-doubling was permitted (protocol-defined criteria, injection volume increased from 0.05 to 0.1 ml and remained at 0.1 ml thereafter). Efficacy (BCVA and CRT) and safety were compared between pooled ranibizumab and sham arms using the full analysis set ( n = 151, patients receiving ≥1 injection).
RESULTS
At month 12, mean ± SD BCVA improved from baseline by 10.3 ± 9.1 letters with ranibizumab and declined by 1.4 ± 14.2 letters with sham ( P < 0.0001). Mean CRT reduction was 194.2 ± 135.1 μm with ranibizumab and 48.4 ± 153.4 μm with sham ( P < 0.0001). Gain of ≥10 letters BCVA from baseline occurred in 60.8% of ranibizumab and 18.4% of sham eyes ( P < 0.0001). Safety data were consistent with previous studies of intravitreal ranibizumab.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema.
- Record: found
- Abstract: found
- Article: not found