- Record: found
- Abstract: found
- Article: found
Clinical Application of Virtual Reality for Upper Limb Motor Rehabilitation in Stroke: Review of Technologies and Clinical Evidence

Read this article at
Abstract
Neurorehabilitation for stroke is important for upper limb motor recovery. Conventional rehabilitation such as occupational therapy has been used, but novel technologies are expected to open new opportunities for better recovery. Virtual reality (VR) is a technology with a set of informatics that provides interactive environments to patients. VR can enhance neuroplasticity and recovery after a stroke by providing more intensive, repetitive, and engaging training due to several advantages, including: (1) tasks with various difficulty levels for rehabilitation, (2) augmented real-time feedback, (3) more immersive and engaging experiences, (4) more standardized rehabilitation, and (5) safe simulation of real-world activities of daily living. In this comprehensive narrative review of the application of VR in motor rehabilitation after stroke, mainly for the upper limbs, we cover: (1) the technologies used in VR rehabilitation, including sensors; (2) the clinical application of and evidence for VR in stroke rehabilitation; and (3) considerations for VR application in stroke rehabilitation. Meta-analyses for upper limb VR rehabilitation after stroke were identified by an online search of Ovid-MEDLINE, Ovid-EMBASE, the Cochrane Library, and KoreaMed. We expect that this review will provide insights into successful clinical applications or trials of VR for motor rehabilitation after stroke.
Related collections
Most cited references125
- Record: found
- Abstract: found
- Article: found
AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both
- Record: found
- Abstract: found
- Article: found
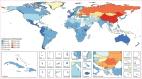
Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016
- Record: found
- Abstract: found
- Article: not found